European Radiolog:原发性肾脏肉瘤你见过吗?来看看都有什么特别的影像学特征
2021-11-20 shaosai MedSci原创
2018年,肾癌占全球所有恶性疾病的2.2%。最常见的肾癌亚型,如透明细胞或乳头状肾细胞癌,均起源于肾上皮细胞。相反,肉瘤是罕见的间质来源的肿瘤,其发病率不到所有肾脏恶性肿瘤的1%。
 2018年,肾癌占全球所有恶性疾病的2.2%。最常见的肾癌亚型,如透明细胞或乳头状肾细胞癌,均起源于肾上皮细胞。相反,肉瘤是罕见的间质来源的肿瘤,其发病率不到所有肾脏恶性肿瘤的1%。尽管最近没有关于肾脏肉瘤的流行病学研究,但来自美国国家癌症数据库和监测、流行病学和最终结果(SEER)数据库的数据表明,肾脏肉瘤的罕见性在肾脏恶性肿瘤中占1%。与非肉瘤类的肾脏肿瘤相比,肾脏肉瘤患者的预后较差,5年总生存率仅为14.5%。
2018年,肾癌占全球所有恶性疾病的2.2%。最常见的肾癌亚型,如透明细胞或乳头状肾细胞癌,均起源于肾上皮细胞。相反,肉瘤是罕见的间质来源的肿瘤,其发病率不到所有肾脏恶性肿瘤的1%。尽管最近没有关于肾脏肉瘤的流行病学研究,但来自美国国家癌症数据库和监测、流行病学和最终结果(SEER)数据库的数据表明,肾脏肉瘤的罕见性在肾脏恶性肿瘤中占1%。与非肉瘤类的肾脏肿瘤相比,肾脏肉瘤患者的预后较差,5年总生存率仅为14.5%。
对于一般的肾脏肿块评估,横断面成像如计算机断层扫描(CT)和磁共振成像(MRI),是初步诊断和治疗计划的基石。特别是对于肾脏肉瘤,有三篇综述文章和许多病例报告对CT和MRI成像特征进行了评估。这些研究描述了肾脏肉瘤特有的一些影像学特征,如囊性增生和中央钙化。然而,这些文献并没有评估这些特定特征的发生概率,也缺乏标准化的影像学评估。
近日,发表在European Radiology杂志的一项研究系统地评估了肾脏肉瘤的影像学特征,并提出了一种准确区分肾脏肉瘤和非肉瘤性肾脏肿瘤的方法,为肾脏肉瘤的准确诊断及治疗评估提供了强有力的参考依据。
本研究评估了1995年至2018年诊断为肾脏肉瘤的成年患者。肾脏肉瘤与非肉瘤的肾脏肿瘤患者相比是1:4。使用21个预定义的成像特征评估了CT/MRI结果。根据人口统计学和影像学特征,训练了一个随机森林模型来预测肾脏肉瘤与非肉瘤肾脏肿瘤。
最终纳入34个肾脏肉瘤,并与136个非肉瘤肾脏肿瘤进行比较。肾肉瘤患者跟为年轻(中位数55岁 vs 67岁,P<0.01),而且表现更复杂(RENAL高分复杂度79.4% vs 25.7%,P<0.01)。与非肉瘤的肾脏肿瘤相比,肾脏肉瘤体积更大(中位直径108 vs. 43毫米,p < 0.01)、形状不规则、边缘不清晰、更常表现出肾静脉或下腔静脉的侵犯、肿瘤坏死、直接侵犯邻近器官以及与肾动脉或静脉的包绕(p < 0.05)。随机森林算法预测肾肉瘤组织学的中位AUC=93.8%,其敏感性、特异性和阳性预测值分别为90.4%、76.5%和93.9%。肿瘤直径和RENAL评分是识别肾脏肉瘤相关性最强的影像学特征。
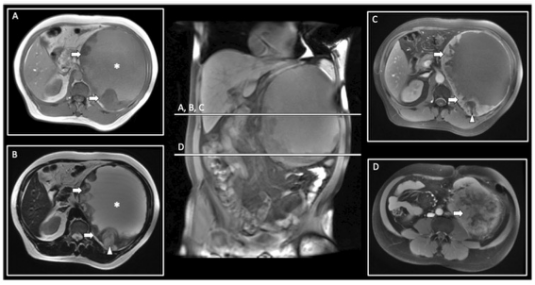
图 49岁男性患者的MRI图像,其左侧肾脏囊性肿块直径为204毫米,并伴有肾脏下移。T1WI(A)显示中等的中心信号强度(SI;星)和低SI的结节边缘(箭头)。T2WI(B)显示高SI中心囊肿(星)以及结节边缘(箭头)内的坏死成分(箭头)。增强后的T1WI脂肪饱和成像(C,D)证实结节边缘(箭头)增强,有坏死成分(箭头),左肾上极表现为肿块状(箭头,D)。组织病理学分析显示,肾脏骨肉瘤的中心囊状物具有肌样内容,壁上有坏死区,并有骨质和软骨成分。
肾肉瘤是罕见的肾脏间质肿瘤,往往表现为年轻患者的大而复杂的肾脏肿块。根据标准化的影像学特征和患者人口统计学训练的随机森林算法显示,使用交叉验证法对肾脏肉瘤和非肉瘤肾脏肿瘤的区分具有良好的诊断准确性。肿瘤直径和RENAL评分是识别肾脏肉瘤最相关的影像特征。这种算法有助于在临床实践中及时和准确地诊断肾脏肉瘤,以优化肾癌患者的治疗并其个体化成为可能。
原文出处:
Johannes Uhlig,Annemarie Uhlig,Sophie Bachanek,,et al.Primary renal sarcomas: imaging features and discrimination from non-sarcoma renal tumors.DOI:10.1007/s00330-021-08201-4
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#原发性#
37
#PE#
28
学习
56
谢谢!
59
坚持学习
59