简易法经脐单孔腹腔镜治疗剖宫产瘢痕部位妊娠5例报道
2019-07-25 杜欣 刘玉兰 冯同富 实用妇产科杂志
近年来随着剖宫产率的增加以及对剖宫产瘢痕 部位妊娠( cesarean scar pregnancy, CSP) 认识程度的 加深,其发病率呈上升趋势。目前治疗方式繁多[1~3], 但无统一治疗方案,而文献认为应根据 CSP 分型不 同,采用不同的治疗方式[4]。腹腔镜治疗部分Ⅱ型及 Ⅲ型 CSP,取得满意效果[4~6]。经脐单孔腹腔镜目前 已应用于外科和妇科临床[7, 8],安全性和有效性已得
近年来随着剖宫产率的增加以及对剖宫产瘢痕 部位妊娠( cesarean scar pregnancy, CSP) 认识程度的 加深,其发病率呈上升趋势。目前治疗方式繁多[1~3], 但无统一治疗方案,而文献认为应根据 CSP 分型不 同,采用不同的治疗方式[4]。腹腔镜治疗部分Ⅱ型及 Ⅲ型 CSP,取得满意效果[4~6]。经脐单孔腹腔镜目前 已应用于外科和妇科临床[7, 8],安全性和有效性已得 到证实,在妇科领域单孔腹腔镜已在恶性肿瘤手术中 得以尝试[9, 10],但是单孔腹腔镜切除 CSP 病灶并行子 宫修补文献报道较少。本文就 5 例单孔腹腔镜治疗CSP 情况进行病例报道及分析。
1 资料与方法
1. 1 一般资料 收集 2018 年 2 月至 2018 年 5 月在 湖北省妇幼保健院住院的 5 例进行经脐单孔腹腔镜 下 CSP 病灶切除加子宫下段修补术病例,平均年龄 32. 20±3. 11 岁,平均停经 56. 20±10. 33 天,平均孕次 3. 60±1. 34 次,平均产次 1. 20±0. 45 次,术前血 β-人 绒毛膜促性腺激素( β-hCG) 为 25248. 16±29158. 15 U/L。见表 1。
1. 2 CSP 诊断与分型 根据 2012 年国内向阳教授提 出的分型[11]: Ⅰ型: 宫腔内孕囊存活型; Ⅱ型: 瘢痕处 肌层内孕囊型; Ⅲ型: 包块型或类滋养细胞疾病型。 该文 5 例中Ⅱ型 2 例,Ⅲ型 3 例。
1. 3 术前止血预处理 术前 24~72 小时给予双侧子 宫动脉甲氨蝶呤( MTX) 共 75 mg 灌注和明胶海绵颗 粒栓塞,进行止血预处理。
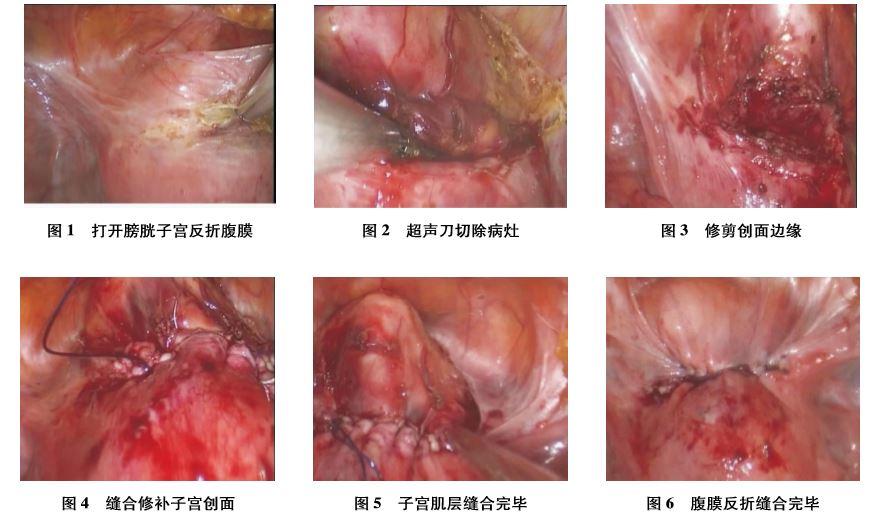
1. 4 手术方式与手术步骤 手术方式采取全身麻醉 下简易法经脐单孔腹腔镜 CSP 切除+子宫下段修补 术。手术步骤: ①全身麻醉后患者置于截石位,留置 导尿,不用举宫器,经脐做 2. 5 cm 纵切口,进入腹腔, 置入切口保护套,套上手套,并翻转套合紧密。于 3 个手指尖剪开手套,置入戳卡,缝线固定,自制简易入 路平台完成。②建立气腹。主要手术器械: 10 mm、 0°腹腔镜( 德国卡尔史托斯公司) ,普通的腹腔镜器械 ( 杭州康基医疗器械有限公司) ,双极电凝( 杭州康基 医疗器械有限公司) ,超声刀( 美国强生 Harmonic) 等, 未使用前段弯曲腹腔镜器械。置镜后观察盆腹腔,台 下子宫颈钳钳夹子宫颈( 不上举宫器) ,举起子宫颈 后,使子宫颈峡部病灶面向手术者。③如术前未行止 血预处理,可向宫体注射垂体后叶素 6 U。④超声刀 剪开膀胱子宫反折腹膜( 见图 1) ,充分分离膀胱子宫 颈间隙,尤其是两侧宫旁,充分暴露瘢痕部位妊娠病 灶。⑤病灶暴露充分后,剪刀或超声刀清除妊娠病灶 组织( 见图 2) ,剪刀修剪创面边缘( 见图 3) ,标本由子 宫颈经阴道取出。若孕囊较大,先行清宫术。⑥缝合时由子宫颈钳钳夹子宫颈,摆动子宫颈,配合缝合。 从腹壁进针,并留线,钳夹固定腹壁外缝线。可从左 侧、右侧或出血多的一侧开始缝合,采取连续缝合法 ( 见图 4) ,单手连续缝合最后拉紧缝线,也可两手逐 针缝合拉紧缝线。一般连续缝合两层,第二层采用褥 式缝合以加厚创面。⑦连续缝合两层后打结( 见图 5) 。⑧缝合腹膜反折,恢复解剖结构( 见图 6) 。⑨缝 合成型肚脐, 2-0 合成线间断缝合腹膜及筋膜 3 针。 脂肪层厚者两侧角部各缝合皮下脂肪层一针,脂肪层 薄者,可以免除该层缝合,直接缝合皮肤层,皮肤层用 4-0 合成线连续皮下缝合,皮肤正中垂直缝至筋膜层, 使肚脐成型,术毕。
2 结 果
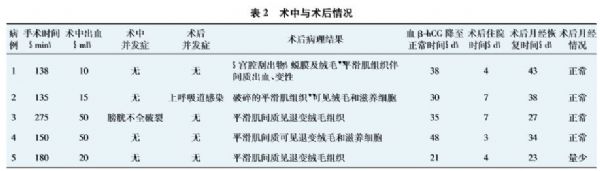
5 例患者中有 3 例术前行子宫动脉栓塞( 例 1、例 3、例 4) ,术前 24~72 小时行右侧股动脉穿刺,双侧子 宫动脉插管,注入甲硝唑 50 ml, MTX 75 mg 和适量直 径约 700~1000 μm 明胶海绵栓塞颗粒。所有患者术中平均出血 29. 00±19. 49 ml,手术平均用时 175. 60± 58. 35 分钟,术后住院 5. 00±1. 87 天,术后血 β-hCG 降至正常时间为 34. 40±9. 97 天,月经恢复正常时间 为 33. 00±8. 09 天。术中出血、手术时间及预后情况 见表 2。随访半年,均未出现其他不适。
3 讨 论
CSP 指有剖宫产史孕妇,胚胎着床于子宫下段剖 宫产切口瘢痕处,是一种特殊部位的异位妊娠,为剖 宫产的远期并发症之一。CSP 可致子宫破裂、大出 血, 严重危害育龄期妇女的健康及生育能力。随着剖 宫产率的不断上升, CSP 作为剖宫产的远期并发症, 逐渐引起重视。早期诊断、早期治疗 CSP 对保护育龄 期妇女的生育能力及生命健康具有重要意义。 CSP 治疗方法的选择主要依靠其分型、病灶大小 及血 β-hCG 的高低[4],对于部分Ⅱ型和Ⅲ型的病例, 手术切除病灶的同时进行子宫修补是最终治疗选 择[4~6]。虽然腹腔镜对操作技术要求高,但因为微创 广受患者和医生喜爱,而且技术的普及,使得腹腔镜 手术治疗 CSP 已成为常见方式。近年来,由于年轻女 性爱美需求增加,又使单孔腹腔镜技术在妇科得到逐 步应用,故本报道结合 5 例简易法经脐单孔腹腔镜治 疗 CSP 进行总结。 3. 1 经脐单孔腹腔镜手术优势和劣势 单孔腹腔镜 由于操作者失去操作三角,同时镜头方向与操作手臂 平行,视线容易被阻挡,操作难度增加,而缝合和打结 被认为是单孔腹腔镜的难点。CSP 病灶位于宫颈峡 部,更增添腹腔镜缝合难度,单孔腹腔镜下缝合更是 难上加难。单孔腹腔镜把伤口隐藏在皱褶的肚脐里, 形似“无痕”,较多孔腹腔镜更微创,大受患者好评。 3. 2 经脐单孔腹腔镜治疗 CSP 的体会要点 ①由于 CSP 病灶位于宫颈峡部,手术野不易暴露清楚,不用 举宫器,仅仅使用子宫颈钳钳夹子宫颈,使子宫颈朝 上,宫底朝下,子宫峡部病灶面向手术者,更利于手术 创面的暴露。这是手术成功的基本保证。②由于单 孔腹腔镜两手配合难度增加,手术难点之一是分离膀 胱子宫颈间隙。由于患者多有 1 次或 2 次剖宫产史, 膀胱与子宫颈界限不清,如果不好辨认,可以灌注膀 胱后找到膀胱界限后再行分离,或从膀胱两侧旁间隙 逐渐向中间部位钝性分离。由于界限疏松,间隙找准 的话很容易分离,配合台下子宫颈位置的移动, 5 例病 例分离过程顺利,无膀胱输尿管损伤。③单孔腹腔镜 下缝合是难点,多数报道缝合伤口采用倒刺线缝合, 而笔者采用常规合成线缝合没有困难。注意尽量选 择大针,譬如 48 mm 长度大针,更利于出针,腹壁吊线 有利于暴露手术野和拉紧缝线,同时子宫颈钳钳夹子 宫颈举宫非常重要,有利于摆动子宫颈,配合另一只 手进针。第一针缝合一侧角时不一定要到位,缝合一 针后,向对侧拉线,第 2 针基本可以到位,注意缝线超 过角部顶端创面约 0. 5 cm,防止术后创面渗血,同时 避免损伤膀胱和输尿管。此次报道的 5 例中,有 1 例 病灶较大,两手配合缝合困难,笔者左手举宫,摆动子宫颈位置,右手单手缝合全部一层后,再逐针拉紧缝 线。也可以左手拉线来摆动子宫位置,配合右手进 针, 出针后,两手轮流拉线至拉紧,交由左手继续拉紧 缝线不松。另外,单孔腹腔镜以上下操作、左右交叉 操作为原则,一定要摒弃多孔腹腔镜操作思路,形成 单孔腹腔镜操作习惯后,手术就变得比较容易了。③ 打结是难点, 可以利用针的弯曲制造操作三角,或利用 腹壁吊线来绕线、 或者利用线的柔软性先绕圈,再将线 头塞过去完成打结。 3. 3 术前止血预处理的重要性 由于 CSP 部位血供 丰富,术前止血预处理非常重要。有研究显示[12, 13], 孕囊直径≥3 cm 时出血风险较大建议行子宫动脉栓 塞( UAE) ,尤其孕囊直径≥5 cm 时大出血风险极高; 还有文献报道[14]: 当Ⅱ型患者孕囊直径≥3 cm 或表 面肌层厚度<0. 2 cm 合并孕囊周边有血流信号时,建 议行子宫动脉栓塞后再清宫或腹腔镜手术或直接开 腹手术。Ⅲ型患者建议行子宫动脉栓塞后再清宫或 直接考虑行开腹手术。该 5 例患者中,有 3 例行子宫 动脉栓塞术,均为包块直径大于 3 cm 或包块表面肌 层缺如或仅 0. 15 cm 厚; 而另 2 例虽然包块表面肌层 不超过 0. 15 cm,但是血 β-hCG 值均较低,所以未行子 宫动脉栓塞处理。 3. 4 5 例手术患者预后分析 5 例患者无一例中转, 除 1 例因为拉线时导致挫伤膀胱浆肌层,造成膀胱不 完全破裂,行镜下缝合以外,余均无其他并发症。患 者术后 3 ~ 7 天出院,未延长住院时间。血 β-hCG 均 于 2 月内降至正常。除 1 例月经量稍少以外,其余 4 例月经恢复正常,其中 1 例原有经期 15 天,术后月经 期缩短至 8~9 天。5 例患者共随访半年,未出现其他 不适。 总之,对于部分Ⅱ型和Ⅲ型的 CSP,经脐单孔腹 腔镜手术可以去除病灶,同时行子宫下段修复,微创、 安全,值得推荐。
参考文献略。
原始出处:
杜 欣,刘玉兰,冯同富,叶常鸿等,简易法经脐单孔腹腔镜治疗剖宫产瘢痕部位妊娠5 例报[J],实用妇产科杂志,2019 ,35 (5)。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#瘢痕部#
27
#简易法#
39
#腹腔镜#
37
#瘢痕#
41
谢谢了,学习
69
学习了
63