AACR 2020:拉罗替尼治疗TRK融合肿瘤的亚组分析
2020-04-29 MedSci MedSci原创
拉罗替尼是FDA获批用于NTRK融合晚期实体瘤患者的首个靶向药
拉罗替尼是FDA获批用于NTRK融合晚期实体瘤患者的首个靶向药
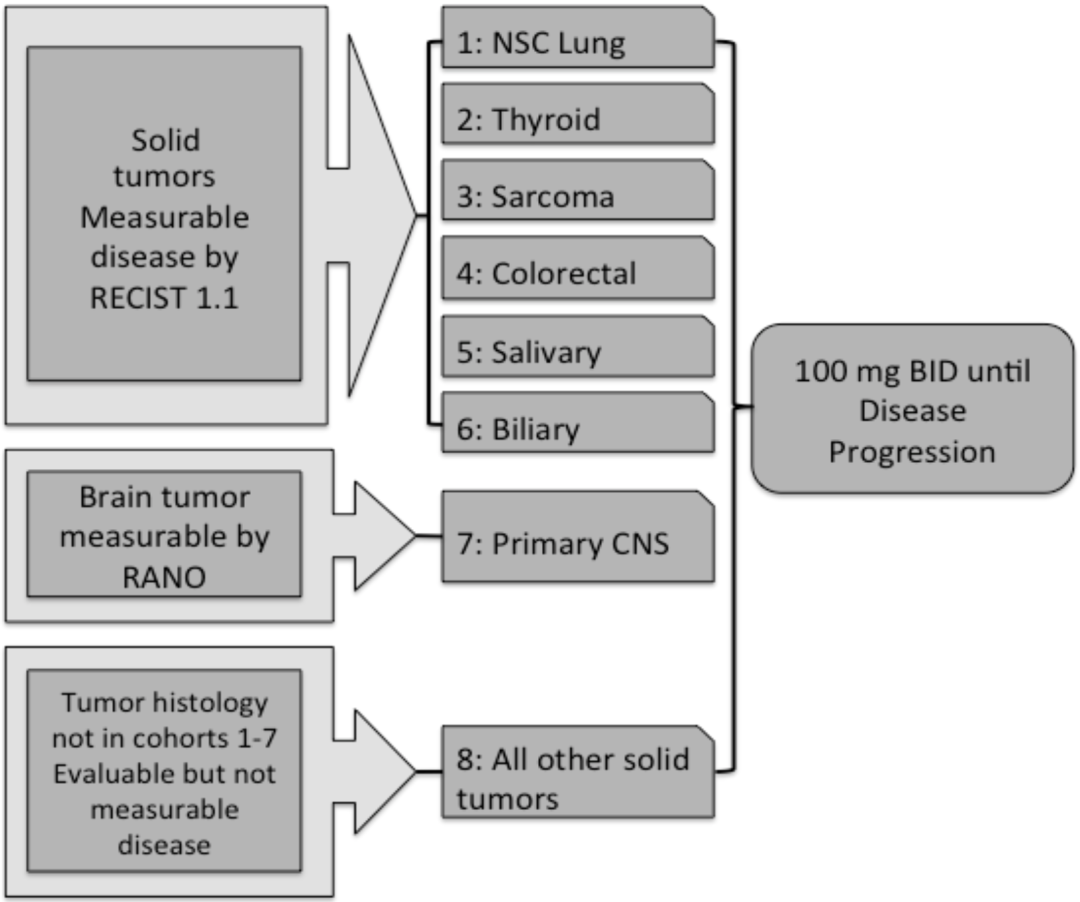
这项研究的分析数据来源于三项临床试验——LOXO-TRK-14001(NCT02122913),SCOUT(NCT02637687)和NAVIGATE(NCT02576431)。研究入组曾接受过标准治疗、具有NTRK基因融合的局部或远处转移的儿童(1个月及以上)或成人的17种实体瘤患者(图2)。主要研究终点是客观缓解率(ORR),次要研究终点是缓解持续时间(DoR)、无进展生存期(PFS)和总生存期(OS)。
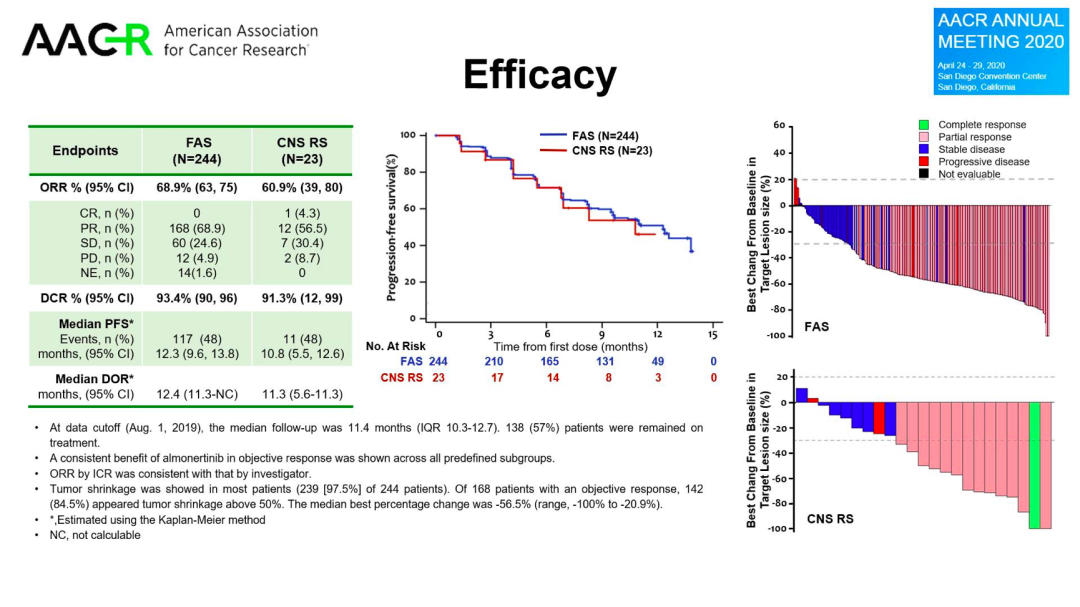
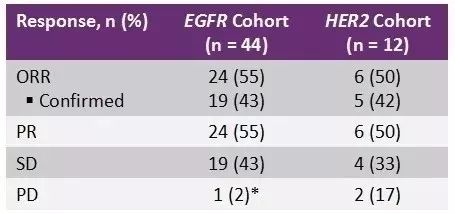
既往数据显示对153例患者的疗效评估结果显示,拉罗替尼使79%(121例)的患者达到客观缓解,其中16%为完全缓解(CR),63%为部分缓解(PR),而无效(PD)患者仅占6%,DOR为35.2个月。在成人和儿童患者间,拉罗替尼的表现也相当一致——成人患者ORR为73%,儿童患者则为92%。12例脑转移患者,其中9例达到疾病缓解,ORR为75%,这与总体人群的79%非常接近,说明拉罗替尼对中枢神经系统转移的实体瘤患者也有效。
此次数据分析了拉罗替尼三项临床试验中根据患者既往治疗线数及ECOG体能评分的疗效。
共分析了159例患者。对于初治的患者,拉罗替尼的ORR最高,可以达到91%,但是随着治疗线数的增加,疗效并没有明显下降,3线及以上治疗的ORR可以维持在85%。ECOG评分方面,体能越好疗效越佳。ECOG PS 0分的ORR为91%,而2分和3分的ORR只有71%和33%。PFS和OS数据在许多亚组都未成熟。

关于拉罗替尼:
拉罗替尼如何发挥抗肿瘤作用呢?神经营养因子受体酪氨酸激酶(NTRK)家族包括 TRKA、TRKB 和 TRKC 三种蛋白,它们分别由NTRK1、NTRK2和 NTRK3 这三种基因编码。NTRK基因融合会导致下游通路,如RAS、PI3K等过度激活,最终结果就是细胞过度增殖导致的肿瘤发生(图1)。而拉罗替尼通过抑制信号通路中的酪氨酸激酶(图1中的“P过程”)来阻断这一过程。多数实体瘤中,均发现NTPK基因融合现象,因此拉罗替尼就能在多种实体瘤中发挥其抗肿瘤作用了。
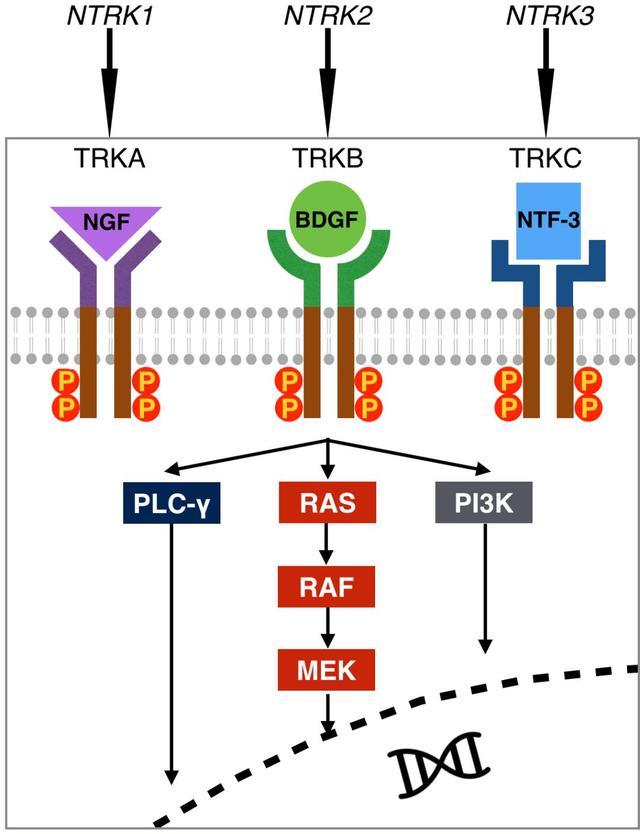
NTRK靶点及下游通路示意图
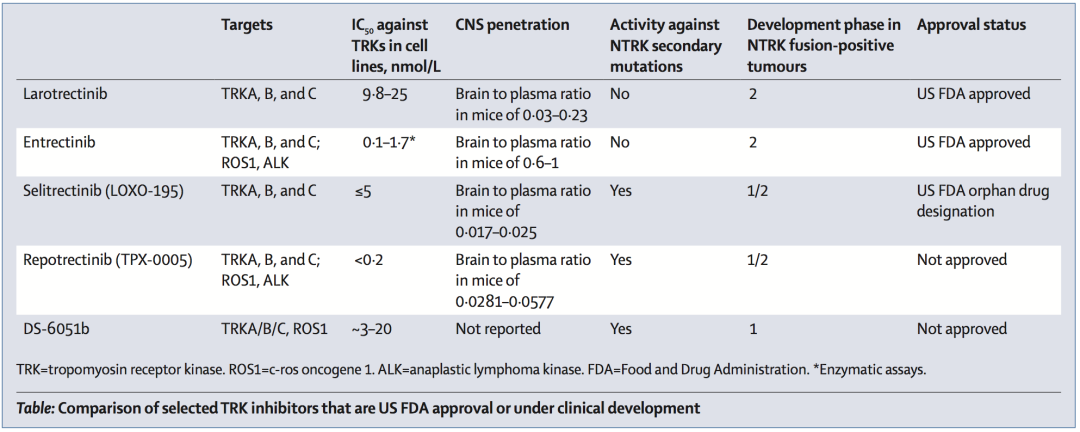
FDA批准及目前正处于研究阶段的TRK抑制剂3
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#TRK融合#
49
#AACR 2020#
28
#ACR#
28
#融合#
33
#AACR#
37