Neurology:高血压、糖尿病、肥胖……贯穿一生的心血管危险因素对晚年认知的影响
2021-03-21 MedSci原创 MedSci原创
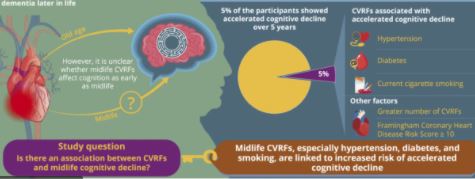
在整个生命过程中,尤其是在成年早期,CVRFs与更大的晚年认知能力下降相关。
目前全世界有近5千万人患有痴呆症,随着社会的老龄化,预计到2050年,老年痴呆人数将增加三倍。目前对于痴呆症,临床上仍然没有有效的治疗方式,所以预防仍然是关键!已有不少研究提示,心血管危险因素(CVRFs)对认知有重要的影响。
去年发表在JAMA Neurol上的一项英国研究提醒:30多岁不注意CVRFs,就开始影响大脑健康了,而且这种年轻时对心脑健康的影响更甚于50岁后。因此呼吁人们,从生命早期就应注重心血管健康,以更有效预防老年痴呆的发生。
目前,人们对早期成人CVRFs和贯穿生命历程的CVRFs如何影响晚年认知能力知之甚少。为了检验整个成人生命过程中的CVRFs与晚年认知变化相关的假设,来自美国加州大学神经精神中心的专家开展了相关研究,结果发表在最新的《神经病学》(Neurology)杂志上。
研究将四个前瞻性队列的数据汇集在一起(n=15001,年龄18-95岁),推算了老年人的体重指数(BMI)、空腹血糖(FG)、收缩压(SBP)和总胆固醇(TC)的轨迹。使用线性混合模型来确定成人早期、中年和晚年CVRFs与晚年整体认知(修改的迷你精神状态检查(3MS))和处理速度(数字符号替代测试(DSST))方面下降的关联。
结果显示,每个时间段的BMI、FG和SBP(而非TC)升高与晚年认知功能衰退更快有关。其中,早年的CVRFs与衰退幅度最大相关,平均10年下降近乎一倍。晚年CVRFs与晚年早期(<80岁)认知的下降相关。在调整所有时间段的CVRFs后,成人早期和晚年CVRFs的关联仍然存在。

因此,糖尿病、高血压、中年肥胖、缺乏体力活动和吸烟等危险因素与血管性痴呆和阿尔茨海默症都有关。结合此前首都医科大学附属北京天坛医院院长王拥军等专家的文章提出,血管因素参与了认知障碍和痴呆的病理生理过程,为通过预防脑血管病来预防痴呆带来了希望。
在整个生命过程中,尤其是在成年早期,CVRFs与晚年认知能力下降幅度更大相关。该研究结果表明,成年早期的CVRFs干预可以使晚年认知受益,但在非常晚年的治疗可能对这些结果没有那么大的帮助。
参考文献:
Yaffe K, et al. Cardiovascular Risk Factors Across the Life Course and Cognitive Decline: <b>A Pooled Cohort Study. Neurology. 2021 Mar 17:10.1212/WNL.0000000000011747.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#血管危险因素#
31
#Neurol#
21
好
68
#心血管危险因素#
25
#心血管危险#
29
受益匪浅
58
谢谢MedSci提供最新的资讯
36
好文章!
50
写得好
69
好
59