Cell Rep:研究发现肿瘤血管新生的新分子标记Apj
2018-11-13 佚名 生物化学与细胞生物学研究所
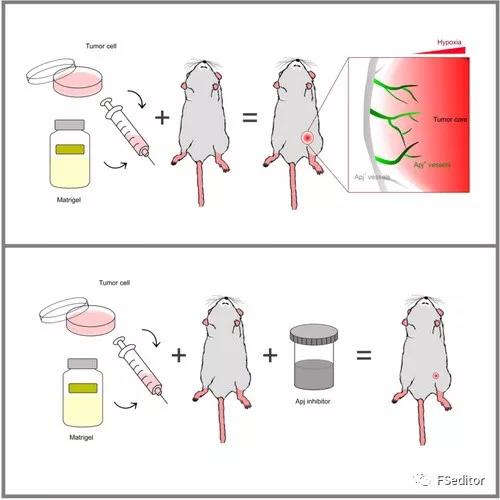
该研究利用在Apj-CreER和Apj-DTRGFP-Luc基因转入小鼠体内分别建立皮下肿瘤移植模型、原位肿瘤移植模型、基因缺陷原位肿瘤模型和化合物诱导肿瘤模型,追踪Apj的表达情况,发现Apj可以特异性地标记大部分的肿瘤新生血管。该研究进一步揭示肿瘤恶性增殖与血管新生的关系,进而加深对肿瘤疾病的认识,同时也为靶向肿瘤新生血管的药物研发提供更加坚实的理论基础。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Cell#
32
#研究发现#
32
#肿瘤血管#
32
#新分子#
35
#血管新生#
39
#CEL#
19
学习咯
62
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
68
了解一下谢谢
55