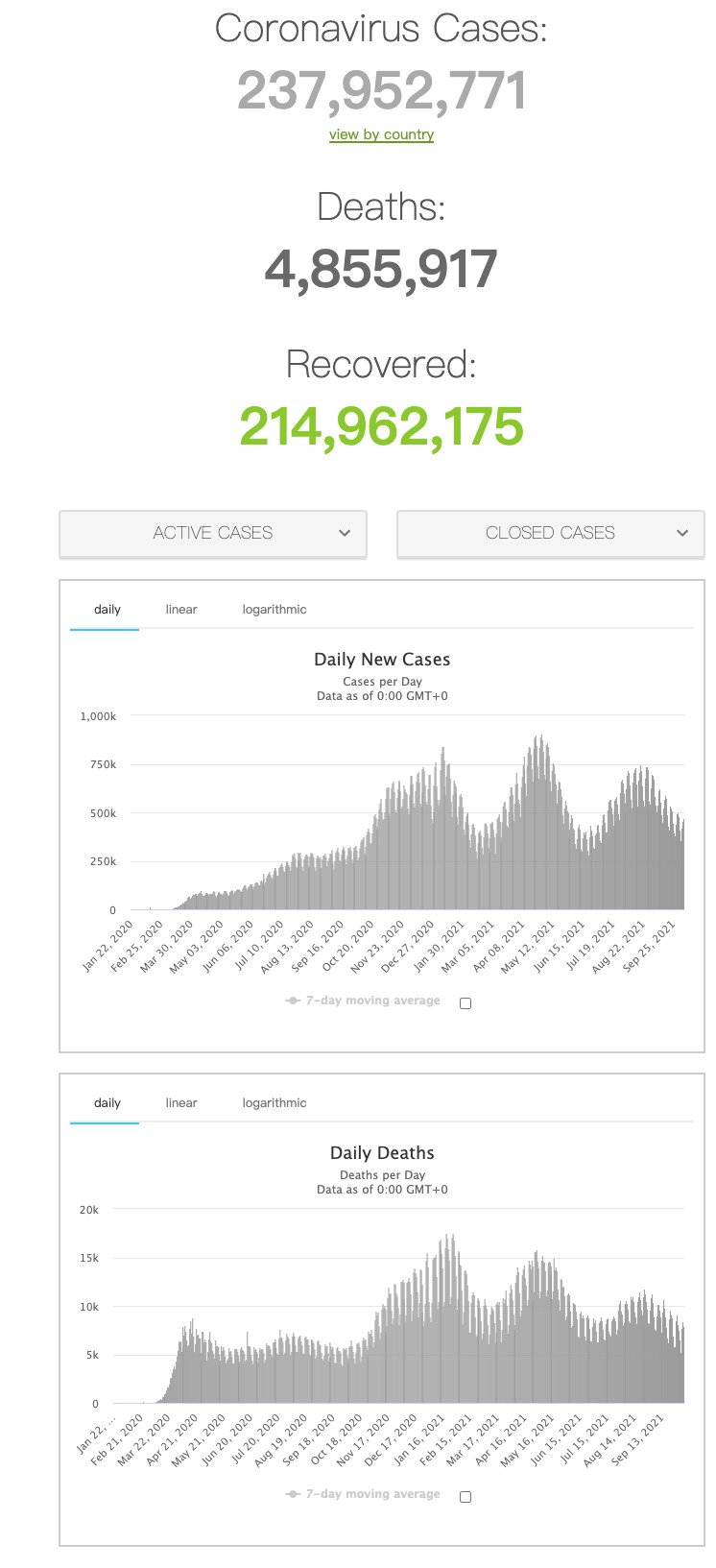
内皮损伤和/或血管周围炎症是COVID-19患者微循环改变和器官损伤的重要发病机制。内皮生物标志物可能不同,包括肾上腺髓质素前体(proADM)和血管内皮素前体(proendothelin),这是反映内皮功能障碍的两种内皮源性标志物,是社区获得性肺炎(CAP)和败血症的预后因素。
发表在Thorax杂志的一篇文章研究了COVID-19急性期患者的内皮生物标志物(proADM和proendothelin)及其与死亡率的相关性。
研究人员采用纵向研究,纳入2020年3月8日至6月4日期间就诊患者400例,其中210例(包括首次住院179例、首次进入ICU(前24小时内)8例和门诊23例)患者在第一天(T1)进行生物标志物分析。其中97例在随访期间(T2)进行生物标志物分析。对照组为无COVID-19感染症状且SARS-CoV-2抗体血清学检查结果为阴性的志愿者。从患者和对照队列抽取外周静脉血,分析proADM和proendothelin,评估内皮损伤。
结果显示,患者T1时proADM和proendothelin水平高于对照组。患者间的proADM和proendothelin水平存在显著差异,门诊患者最低,ICU住院患者最高。对proADM和proendothelin与其他已知新冠肺炎严重程度标志物进行相关性分析发现,与C反应蛋白(CRP)、D-二聚体、乳酸脱氢酶(LDH)呈正相关,与淋巴细胞计数呈负相关。与住院和门诊患者相比,较高的proADM和proendothelin基线水平与病情严重程度和进入ICU治疗相关。第1天proADM或proendothelin水平升高与住院死亡率相关。出院后维持的高水平与弥散能力降低相关。

总之,COVID-19引起proADM和proendothelin增加,反映内皮损伤,出院后可能持续存在。COVID-19诊断时内皮损伤程度与疾病严重程度和预后有关。大多数患者内皮源性标志物持续增加,这与肺一氧化碳弥散量降低有关。
原文出处:
Raúl Méndez, Paula González- Jiménez, et al Acute and sustained increase in endothelial biomarkers in COVID- 19, Thorax, 2021, http://dx.doi.org/10.1136/thoraxjnl-2020-216797.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#标志物#
30
#生物标志#
41
#生物标志#
39
加几分
52