Pediatr Blood Cancer:中性粒细胞减少饮食与食品安全指南对小儿肿瘤患者感染率的有效性
2020-05-31 MedSci原创 MedSci原创
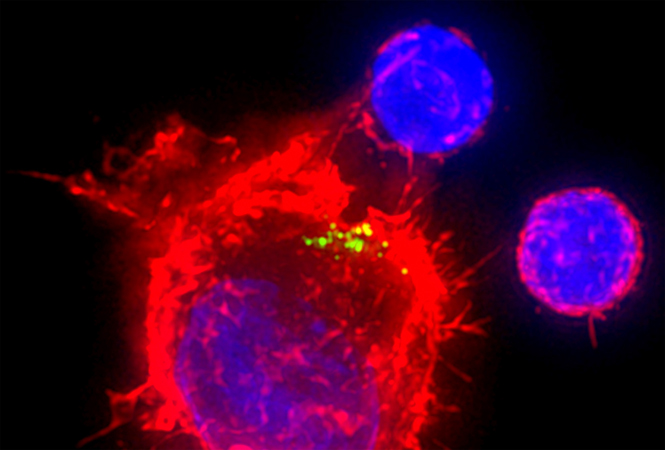
中性粒细胞饮食(ND)是为了避免细菌进入宿主的胃肠道,减少感染。由于缺乏支持ND的证据,小儿肿瘤科医生对ND是否有用仍有争议。这项前瞻性随机对照试验评估了随机接受食品和药物管理局批准的食品安全指南(F
中性粒细胞饮食(ND)是为了避免细菌进入宿主的胃肠道,减少感染。由于缺乏支持ND的证据,小儿肿瘤科医生对ND是否有用仍有争议。这项前瞻性随机对照试验评估了随机接受食品和药物管理局批准的食品安全指南(FSG)与ND加FSG在一个周期化疗期间的儿科肿瘤患者中中性粒细胞感染率的差异。
接受骨髓抑制性化疗的小儿肿瘤患者符合条件。中性粒细胞增多症感染是主要结果,定义为(i)发热伴中性粒细胞增多症或(ii)因临床感染和中性粒细胞增多症入院治疗。中性粒细胞增多症感染率用独立样本的Student's t检验进行比较。通过全面的病历复查确定记录的感染情况,组间采用χ2检验进行比较。
结果显示,150例患者被随机分配到FSG(n = 73)或ND+FSG(n = 77)。最常见的诊断为急性淋巴细胞白血病(32%)和肉瘤(32%)。两组患者发生中性粒细胞感染的比例无明显差异。FSGs 33%与ND + FSGs 35%(P = 0.78)。随机加入ND+FSGs的患者报告称,与单纯服用FSGs的患者相比,遵循饮食疗法需要更多的努力。
综上所述,该研究结果表明,ND对接受骨髓抑制性化疗的小儿肿瘤患者预防感染方面,与FSG相比,ND没有任何益处,患者和家属需要付出更多的努力来坚持。护理癌症患儿的机构应考虑用消炎药指南取代ND指南。
原始出处:
Karen M Moody, Rebecca A Baker, et al., A Randomized Trial of the Effectiveness of the Neutropenic Diet Versus Food Safety Guidelines on Infection Rate in Pediatric Oncology Patients. Pediatr Blood Cancer. 2018 Jan;65(1). doi: 10.1002/pbc.26711. Epub 2017 Jul 11.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#中性粒细胞减少#
34
#PE#
33
#粒细胞减少#
35
#DIA#
42
#中性粒细胞#
37
#肿瘤患者#
35