Clinica Chimica Acta:华北地区不同人群CD36抗原缺乏、血小板同种异体抗体分布及血小板同种异体抗体对妊娠影响?
2019-12-02 gladiator MedSci原创
血小板抗体可导致血小板输血难<span lang="EN-US" style="font-size:12.0pt;mso-bidi-font-size:14.0pt;font-family:"Calibri","sans-serif"; mso-fareast-font-family:宋体;mso-bidi-font-family:"Times
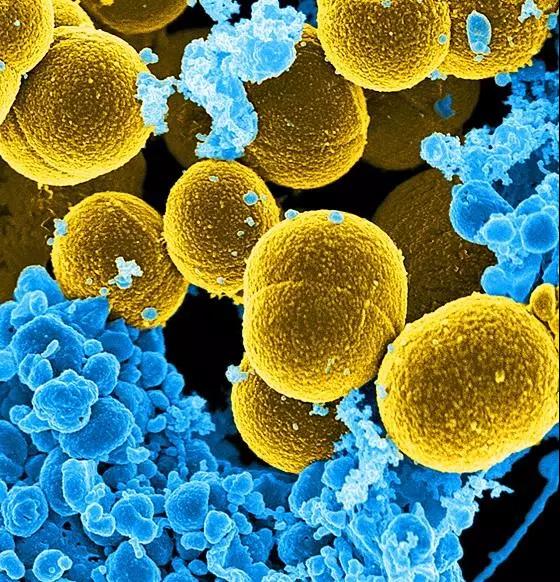
血小板抗体可导致血小板输血难(PTR)、胎儿/新生儿同种免疫性血小板减少(FNAIT)等临床疾病。本研究旨在了解华北地区不同人群CD36表达、血小板同种抗体分布及血小板同种抗体对妊娠的影响。
已进入以通过采集血液病患者、孕妇、献血者等612例受试者全血标本,检测CD36表达,进行血小板抗体筛选及特异性鉴定。为了调查FNAIT的发生,对1552例产科住院孕妇进行回顾性分析。
研究结果显示,CD36缺乏症表达率为2.12%(13/612),所有病例均为II型缺乏症,而未检出I型缺乏症,总体而言,该率低于华南地区(3.43%)、日本(4.87%)和黑人(4.18%),但高于白人(0.09%)。积极的血小板抗体筛选血液病人组(6.86%,14/204)和孕妇组(6.31%,13/206)高于献血者组(0.49%,1/202),P < . 01。在1552名孕妇中,没有儿童患有FNAIT。
研究结果表明,北方地区CD36缺乏的频率较低,均为II型,未检出CD36抗体。推测该人群因CD36缺乏而导致免疫相关血小板减少的风险极低。血液学和多次流产的患者应早期监测血小板抗体。
原始出处:
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#同种异体#
45
#CTA#
23
#CD36#
28
#抗原#
31