颈内动脉海绵窦瘘介入栓塞全麻术中心跳骤停1例
2018-11-15 朱斌斌 陈福贵 曹庆华 介入放射学杂志
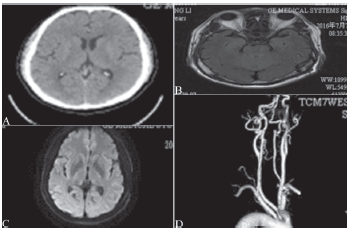
患者女,42岁,因“车祸后视物重影,右眼红,眼突出2个月余”收治入院。体检眼球突出度:右16 mm,左13 mm,右眼各方向活动均受限,球结膜充血,结膜下血管扩张迂曲,角膜透明,对光反应正常。右眼B超提示:右眼轻度玻璃体混浊,右眼眼上静脉扩张。
患者女,42岁,因“车祸后视物重影,右眼红,眼突出2个月余”收治入院。体检眼球突出度:右16 mm,左13 mm,右眼各方向活动均受限,球结膜充血,结膜下血管扩张迂曲,角膜透明,对光反应正常。右眼B超提示:右眼轻度玻璃体混浊,右眼眼上静脉扩张。
头颅CTA三维重建提示:“双侧颈内动脉海绵窦瘘”。入院诊断为创伤性颈动脉海绵窦瘘。择期在全麻下行“右颈内动脉海绵窦瘘介入栓塞术”。患者入院血压125/75 mmHg,心率85次/min。麻醉诱导予静脉推注丙泊酚80 mg,咪唑安定3 mg,芬太尼150 μg,顺式阿曲库胺10mg,阿托品0-5mg后,插入3号SLIPA喉罩,麻醉机行间歇正压通气(intermittent positive pressure ventilation,IPPV)。
麻醉维持采用静脉麻醉,瑞芬太尼3 μg·kg-1·h-1和丙泊酚5 mg·kg-1·h-1持续泵注,血流动力学平稳:血压116~124/60~70 mmhg,心率70~80次/min。用Danmeter(合肥诺和电子科技有限公司批号2015003)监测麻醉深度(Bispectra Index BIS),麻醉深度维持在43~57。在泥鳅导丝导引下将6 F导引导管送到右侧颈内动脉近岩谷段,退出导丝。静脉肝素化后,以0.014英寸微导丝带微导管头端带人海绵窦内,退出微导丝,沿着微导管送入EV3 Axium 10 mm×30 cm弹簧圈(The endovascular company,美国)1枚。
造影复查确认后,继续放置各类大小型号弹簧圈共14枚。造影显示眼静脉、海绵窦、岩下静脉显影明显减少,颈内动脉显影良好。选择合适的Hyperglide 4/20辅助球囊(MTI公司,美国),将导管置入海绵窦窦口人口处,充盈球囊临时阻断窦口,复查造影未见颈内动脉显影。此时血流动力学稳定,血压120/75 mmHg,心率77次/min。遂用10 ml生理盐水冲洗微导管上的对比剂,而后微导管内缓慢注入Onyx溶剂二甲基亚砜(dimethyl sulfoxide,Dmso)0.3 ml,正准备注入预先震荡30 min的Onyx胶时,心率变为44次/min,继而迅速变为直线,血压测不出。
予胸外按压的同时,给予阿托品O.5 mg。1 min后窦性心率恢复,42次/min,继续给予阿托品0.5 mg,3 min后心率变为82次/min,血压133/65 mmHg。整个抢救过程,麻醉深度BIS无明显变化。病性改变考虑DMSO毒性。释放球囊,待血流动力学稳定后,缓慢注入Onyx18胶。再次释放球囊造影显示:右侧眼静脉引流已经基本消失,海绵窦、岩下窦显影明显减少,颈内动脉显影良好。结束手术患者苏醒后拔喉罩送入ICU。生命体征平稳,双侧瞳孔等大,对光反应灵敏。
原始出处:
朱斌斌, 陈福贵, 曹庆华. 颈内动脉海绵窦瘘介入栓塞全麻术中心跳骤停1例[J]. 介入放射学杂志, 2017, 26(2):127-128.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#全麻术#
45
#全麻#
42
#心跳骤停#
39
#颈内动脉#
62