Int J Mol Sci:肌肉侵入性膀胱癌中,预测基于放化疗的膀胱保留疗法临床结果生物标记研究
2018-09-25 AlexYang MedSci原创
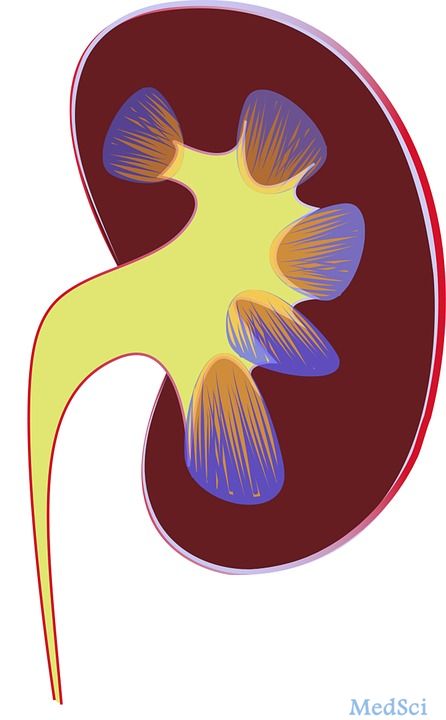
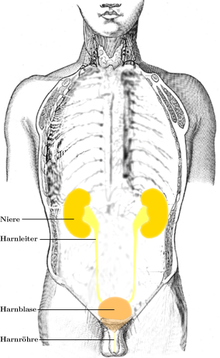
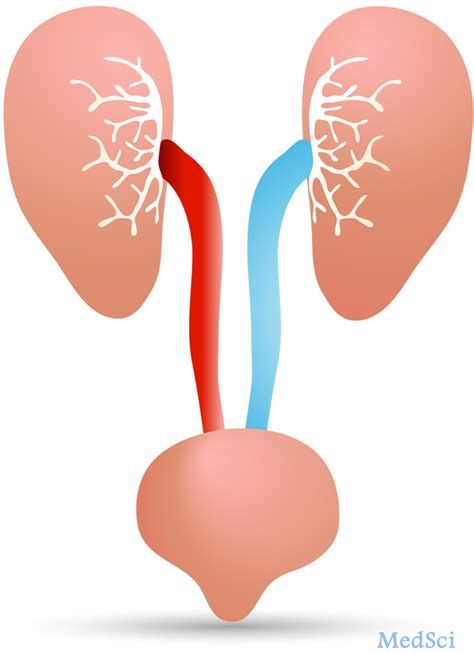
基于放化疗的膀胱保留疗法(BPT)是目前的一种对非转移肌肉侵入性膀胱癌(MIBC)的有效的疗法,并且风险小,同样也是不适用根治性膀胱切除术患者的一种选择。在BPT中,只有那些放化疗后获得完整响应(CR)的患者才有良好的预后和生活品质,并且膀胱功能保留。因此,预测CR和有利的预后对选择BPT患者是非常重要的。最近,有研究人员对预测基于放化疗的BPT临床结果得生物标记进行了回顾。研究人员将研究的生物标
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#临床结果#
22
#侵入性#
36
#放化疗#
29
#生物标记#
30
了解一下,谢谢分享!
72
走资
62