Liver Int:生长分化因子15预测NAFLD患者进展期肝纤维化
2017-09-20 MedSci MedSci原创
总之,研究表明,GDF15可以作为进展期肝纤维化的一种新的生物标志物。
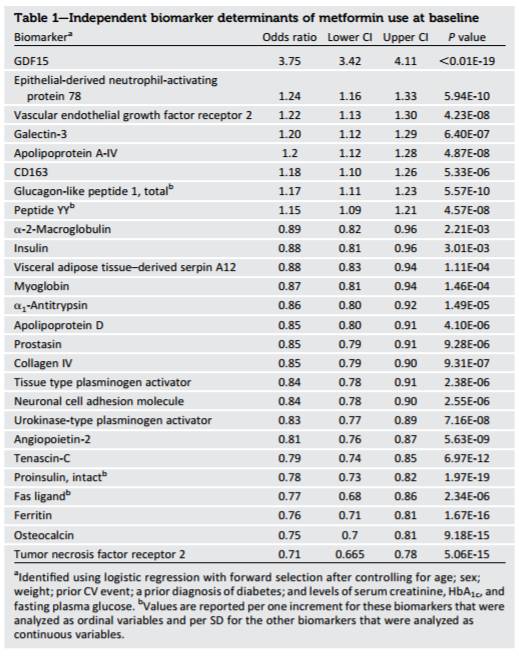
本研究旨在探究生长分化因子15(GDF15)能否独立于胰岛素抵抗,影响非酒精性脂肪性肝病(NAFLD)组织学严重程度。
在经肝组织活检验证的NAFLD队列,研究者使用酶联免疫吸附方法检测血清GDF15水平。
研究结果表明,在190例患者中(平均年龄为53±14岁,男性为52.1%),72例患者(男性, 65.3%)经肝组织活检确定为非酒精性脂肪性肝病(NAFL)患者,78例(男性, 44.9%)患者经肝组织活检确定为非酒精性脂肪性肝炎(NASH)患者。NASH患者的GDF15水平明显高于对照组(P = 0.010)或NAFL患者(P = 0.001)。进展期肝纤维化患者(≥F3)其血清GDF15水平显著高于其他患者(F0-2,P <0.001)。在NAFLD患者中,在没有纳入NASH风险的情况下,即使调整年龄、性别、体重指数、吸烟状况、高血压、糖尿病、天冬氨酸转氨酶、血小板、白蛋白、胰岛素抵抗和低骨骼肌质量等因素(优势比,4.27;95%置信区间,1.04 - 17.63),GDF15水平最高的四分之一仍与进展期肝纤维化显著相关。GDF15水平与肝硬度呈显著正相关(Spearman's rho, 0.525; P < 0.001)。棕榈酸酯治疗显著提高了Kupffer细胞 GDF15 mRNA的表达水平,然而,肝细胞的表达水平并未显著增加。GDF15治疗导致LX-2细胞 a-平滑肌肌动蛋白,I型胶原,磷酸化水平的Smad2和Smad3表达增加。
总之,研究表明,GDF15可以作为进展期肝纤维化的一种新的生物标志物。
原始出处:
Koo B, Um SH, Seo DS, et al. Growth differentiation factor 15 predicts advanced fibrosis in biopsy-proven non-alcoholic fatty liver disease. Liver Int, 2017, Sep 12. doi: 10.1111/liv.13587.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#进展期#
35
#生长分化因子15#
40
#肝纤维#
23
#AFLD#
23