JACC:证据来了——美托洛尔改善肥厚型心肌病患者梗阻症状,并提高生活质量!
2021-12-21 MedSci原创 MedSci原创
与安慰剂相比,美托洛尔在最大运动能力保持不变的前提下,减少了阻塞性HCM患者在休息和运动时的LVOT梗阻,缓解了症状,并改善了生活质量。
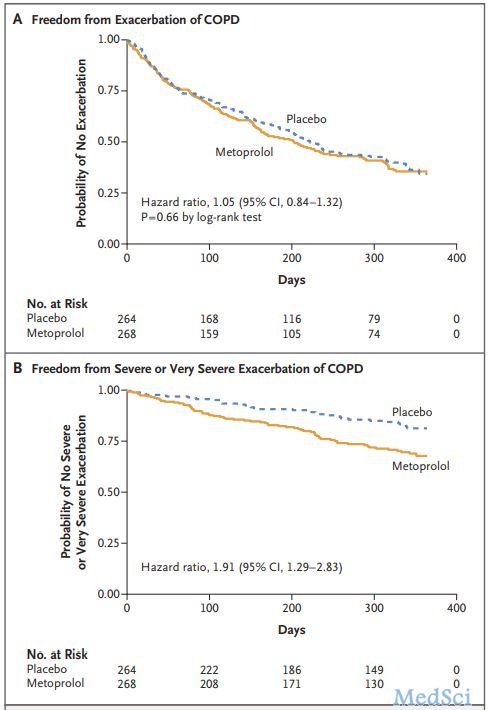
β受体阻滞剂是治疗冠心病的基石,若无禁忌症所有患者均应长期使用。美托洛尔,是临床常用的一种选择性的β1受体阻滞剂。其中,普萘洛尔是一种非选择性的β受体阻滞剂。美托洛尔、比索洛尔、阿替洛尔对β1受体的亲和力大于β2受体的亲和力,因此是选择性的β受体阻滞剂。
非选择性β受体阻滞剂同时阻断β1和β2受体,容易引起支气管痉挛;选择性β受体阻滞剂则主要阻断β1受体,对支气管副作用极少。因此倍他乐克可以用于治疗COPD病人,但哮喘病人禁用β受体阻滞剂。
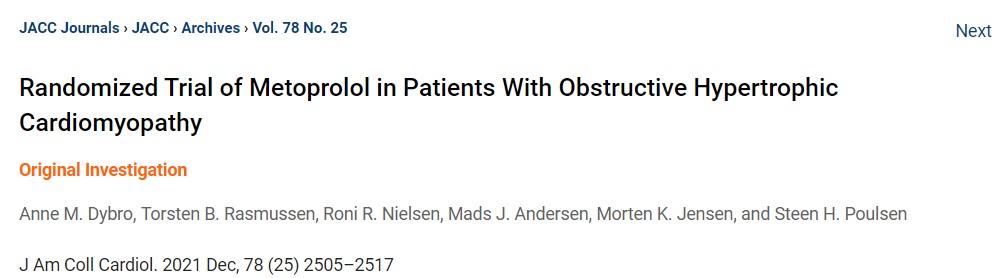
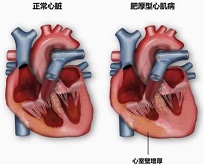
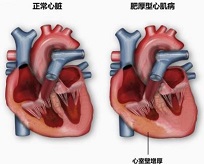
为了研究美托洛尔对阻塞性肥厚型心肌病(HCM)患者的左心室流出道(LVOT)梗阻、症状和运动能力的影响,来自丹麦奥胡斯大学医院心脏病学的专家开展了相关研究,结果发表在JACC杂志上。
这项双盲、安慰剂对照、随机交叉试验于2018年5月至2020年9月招募了29名阻塞性HCM和纽约心脏协会(NYHA)功能分级II级以上症状的患者。患者按随机顺序接受美托洛尔或安慰剂,连续2周。效果参数为LVOT梯度、NYHA分级、加拿大心血管协会(CCS)心绞痛分级、堪萨斯城心肌病问卷总分(KCCQ-OSS),以及心肺运动测试。
结果显示,与安慰剂相比,美托洛尔的LVOT梯度在休息时较低(25 mmHg,IQR:15-58 mmHg vs 72 mmHg,IQR:28-87 mmHg;P = 0. 007),同时在运动高峰期(28 mmHg,IQR:18-40 mmHg vs 62 mmHg,IQR:31-113 mmHg;P<0.001)以及运动后(45 mmHg,IQR:24-100 mmHg vs 115 mmHg,IQR:55-171 mmHg;P<0.0001)也更低。
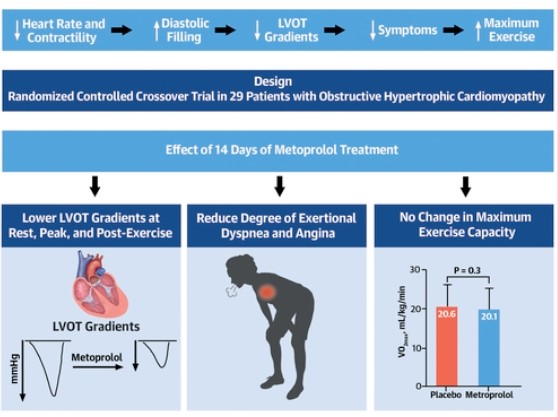
文章图形摘要
在治疗期间,美托洛尔组和安慰剂组分别有14%与38%(P < 0.01)的患者处于NYHA III级或以上。同样,在美托洛尔治疗期间,没有患者处于CCS III级或以上,而接受安慰剂治疗的患者为10%(P < 0.01)。这些发现被美托洛尔治疗期间较高的KCCQ-OSS所证实(76.2±16.2 vs 73.8±19.5;P = 0.039)。
综上,与安慰剂相比,美托洛尔在最大运动能力保持不变的前提下,减少了阻塞性HCM患者在休息和运动时的LVOT梗阻,缓解了症状,并改善了生活质量。
Randomized Trial of Metoprolol in Patients With Obstructive Hypertrophic Cardiomyopathy.
J Am Coll Cardiol. 2021 Dec, 78 (25) 2505–2517
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#JACC#
33
#ACC#
43
#美托洛尔#
50
#肌病#
45