Anesth Analg:胸腔镜手术后行奇静脉水平膈神经阻滞与对照组治疗后同侧肩痛的疗效比较:一项随机对照试验
2021-08-24 “ 罂粟花”公众号 “ 罂粟花”公众号
同侧肩痛(ISP)是肺部手术后的常见问题。我们假设在手术操作位置附近的奇静脉水平处进行膈神经阻滞(PNB)可有效降低ISP。本研究的主要目的是评估PNB对胸腔镜手术(VATS)后ISP的影响。
背景
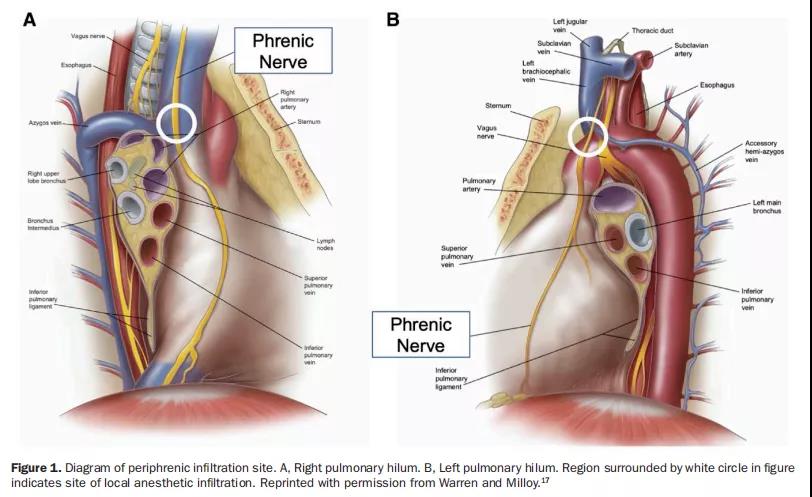
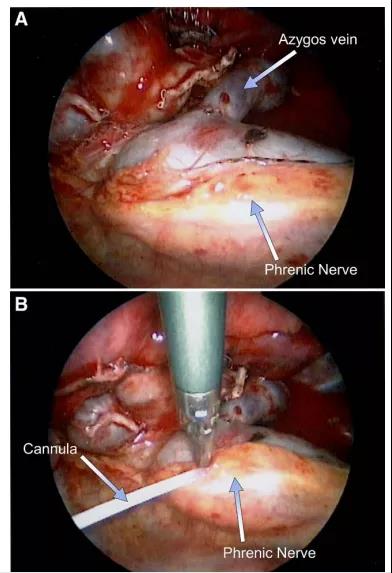
同侧肩痛(ISP)是肺部手术后的常见问题。我们假设在手术操作位置附近的奇静脉水平处进行膈神经阻滞(PNB)可有效降低ISP。本研究的主要目的是评估PNB对胸腔镜手术(VATS)后ISP的影响。
方法
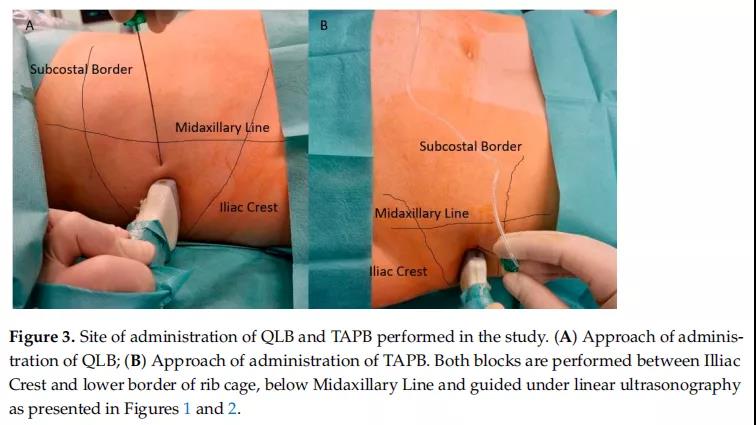
这项前瞻性、随机、患者盲法、单机构试验在大学医院医疗信息网(UMIN000030464)上注册。入组的患者在硬膜外镇痛全身麻醉下行胸腔镜手术。我们将患者随机分配到接受10ml 0.375%罗哌卡因(PNB组)或0.9%生理盐水(对照组),即在胸腔闭合前进行奇静脉水平的同侧膈神经阻滞。术后2、4、8、16和24小时患者静息时ISP使用数字评分量表(NRS,0-10)进行评估。ISP的发生率定义为术后24小时内至少报告一次NRS评分≥1的患者比例。在主要分析中,我们使用了χ2检验来比较PNB组和对照组之间ISP患者的比例。我们观察了患者24小时内ISP的NRS值和术后切口疼痛,以及术后镇痛药的使用频率。并在ISP评估时使用NRS评估患者切口疼痛。最后,我们还评估了患者术后恶心呕吐和肩部运动障碍的发生率。
结果
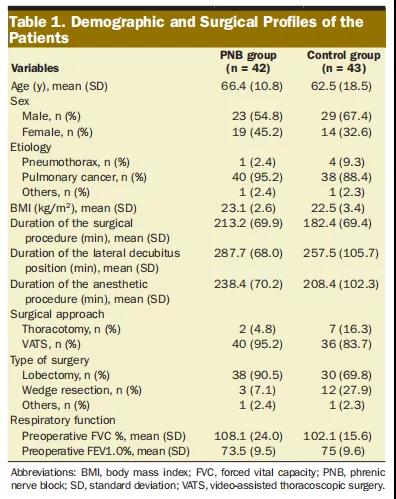
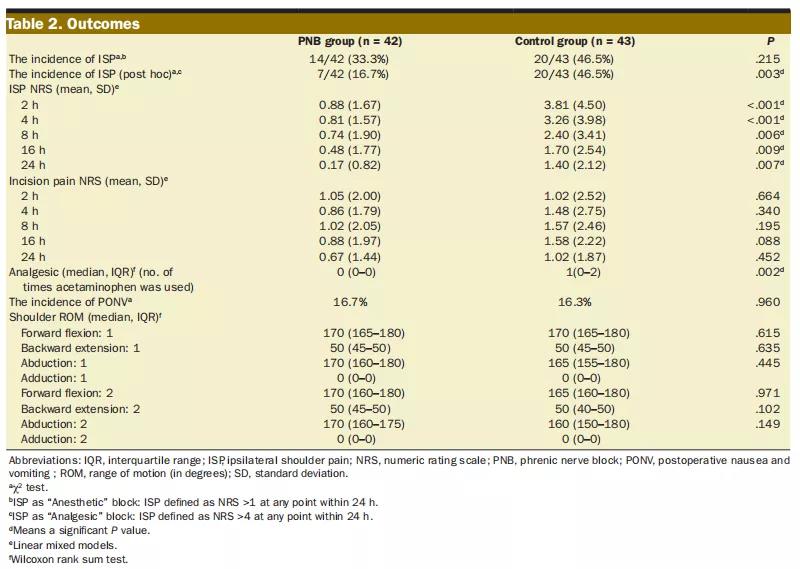
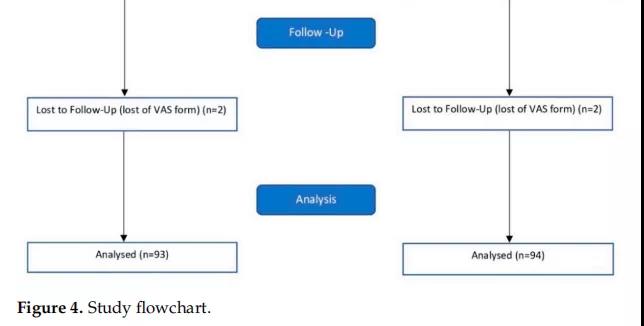
本研究纳入了85例患者,随机分配到PNB组(n = 42)或对照组(n = 43)并对其进行数据分析。两组之间的人口统计学和手术概况没有临床相关差异。ISP的发生率无显着差异(对照组20/43 [46.5%]与PNB组14/42[33.3%];P =0.215)。PNB组ISP的严重程度低于对照组(线性混合效应模型,主要治疗结果[组]:P < 0.001)。两组术后切口疼痛无显着差异。对照组术后镇痛药使用频率显着高于PNB组(Wilcoxon秩和检验,P <0.001)。两组术后恶心和呕吐无显着差异且肩关节活动范围无变化。


结论
奇静脉水平PNB对VATS后ISP的发生率无明显影响。
原始出处:
Kaori Kimura Kuroiwa, Yuki Shiko, Yohei Kawasaki, et al. Phrenic Nerve Block at the Azygos Vein Level Versus Sham Block for Ipsilateral Shoulder Pain After Video-Assisted Thoracoscopic Surgery: A Randomized Controlled Trial.[J]. Anesth Analg 2021;132:1594–602.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ANA#
32
#静脉#
26
#胸腔镜手术#
37
#膈神经#
32
#EST#
24
#Anal#
49
#对照组#
53
#对照试验#
25
#对照#
25
#随机对照试验#
30