J Int AIDS Soc:HPTN 071(PopART)试验中通过横断面发病率分析对人群水平HIV-1发病率进行估计
2022-01-07 从医路漫漫 MedSci原创
艾滋病毒发病率是人口中艾滋病毒新感染率,是评估疫情状况和预防干预措施有效性的主要措施。横断面发病率分析使用试验算法(MAAs)来估计艾滋病毒发病率。
背景:艾滋病毒发病率是人口中艾滋病毒新感染率,是评估疫情状况和预防干预措施有效性的主要措施。横断面发病率分析使用试验算法(MAAs)来估计艾滋病毒发病率。与使用纵向队列研究估算发病率相比,这种方法更简单,成本更低。目前,行业标准和最广泛使用的发病率估计测试算法,包括人口健康指标评估(PHIA)和用近期测定法跟踪控制流行(TRACE),是限制抗原活性测定加病毒载量(LAg+VL)。在抗逆转录病毒治疗覆盖率和病毒抑制水平较高的情况下,评估准确性的数据有限。了解这些环境下的横断面发病率估计很重要,因为病毒抑制可能导致最近的测试结果错误。我们比较了多试验算法(MAA)与社区随机HPTN 071 (PopART)试验中观察到的发病率估计的准确性,在该试验中,大多数HIV感染参与者受到病毒抑制。
方法:在研究的第二年对HIV发病率进行评估,只包括在研究开始后1年和2年(2016-2017)就诊时接受HIV检测的个人。将三种MAA的发病率估计值与1-2年的观察发病率进行比较(MAA-C:LAG-Avidity<2.8ODN+BioRad亲和力指数<95%+VL>400拷贝/ml;LAG+VL MAA:LAG-AVIDITY<1.5ODN+VL>1000拷贝/ml;Rapid+VL MAA:Asanté近期快速结果+VL>1000拷贝/ml)。三种MAA的平均近期感染持续时间(MDRI)分别为248、130和180天。
结果:这项研究包括15845名HIV阴性的人,4406名在两次访问中都呈HIV阳性的人,以及221名在两次访问之间进行血清转换的人。在为期两年的访问中,所有HIV阳性参与者的病毒载量(VL)数据都是可用的。64名(29%)血清转换者和3227名(72%)患者出现病毒抑制(<400拷贝/ml)。观察HIV感染率为1.34%(95%CI:1.17~1.53)。估计发病率与观察到的发病率相似,MAAC为1.26%(95%CI:1.02-1.51),LAG+VL MAA为1.29(95%CI:0.97-1.62)。用Rapid+VL MAA估计的发病率显著低于观察发病率(0.92%,95%CI:0.69-1.15,p<0.01)。

图1 HPTN 071中横断面发病率估计值与观察发病率的比较(PopART)。该图显示了在HPTN 071(PopART)试验中观察到的HIV年发病率与用三种多分析算法(MAAS)估计的发病率的比较。缩写:LAG,极限抗原亲和力测定;MAA-C,Clade C多重测定算法;Rapid,Asante快速滞后试验;VL,病毒载量。
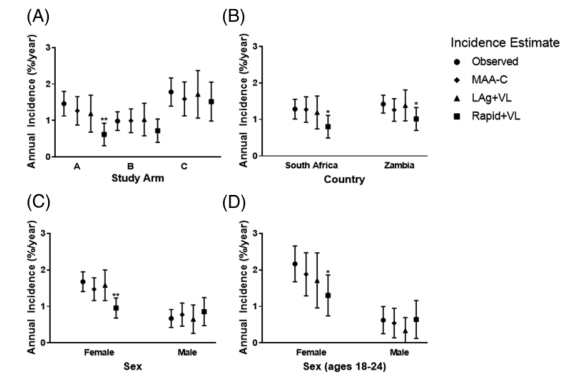
图2 青年人HPTN 071 (PopART)的横断面发病率估计与观察发病率的比较,按研究机构、国家、性别和性别分列。图中显示了三种多试验算法(MAAs)的观察发病率和发病率估计。圆表示根据纵向随访观察到的发病率。子分析由研究小组(a)提出;国家(b);性(c);青少年(18-24岁)的性别(d);95%的置信区间显示为每个点估计发病率。与观察到的发生率有显著差异的发生率估计是值得注意的(* p<0.05;* * p < 0.01)。缩写:LAg,限制性抗原活性测定;MAA-C, Clade C优化的多分析算法;Asante快速LAg检测法;VL,病毒载量。
结论:MAA-C和LAG+VL MAA在病毒抑制水平较高的队列中提供了准确的发生率点估计。Rapid+VL显著低估了发病率,这表明制造商推荐的MDRI过长,或者该检测方法不够准确地检测最近感染。
原文出处:
Klock E, Wilson E, Fernandez RE,et al.Validation of population-level HIV-1 incidence estimation by cross-sectional incidence assays in the HPTN 071 (PopART) trial.J Int AIDS Soc 2021 Dec;24(12)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PTN#
42
#发病率#
39
#横断面#
47
#AID#
44
#ART#
37
#AIDS#
0