JAMA Pediatr:硬膜外镇痛与后代自闭症谱系障碍风险
2021-04-28 MedSci原创 MedSci原创
硬膜外镇痛不会增加后代自闭症谱系障碍风险

自闭症谱系障碍(ASD)是一种广泛性发育障碍,其病征包括异常的语言能力、交往能力、兴趣爱好以及固执行为等,多发病于幼儿早期。统计发现,美国2002年ASD发病率仅为0.66%,而2016年增长至1.85%。围产期疾病和不当的干预措施,包括出生损伤、出生低体重和剖宫产,会增加新生儿神经系统发育异常风险,可能与ASD风险相关。过去的20年里,硬膜外镇痛(ELA)是用于分娩镇痛的最为常用的方法。近日研究人员考察了硬膜外分娩镇痛对后代患自闭症谱系障碍风险的影响。
研究人员收集了加拿大马尼托巴省卫生保健数据库数据,包含2005年至2016年出生的单胎阴道分娩活产新生儿数据,按照是否接受了ELA分层,随访持续至2019年。研究的主要终点为ASD诊断。
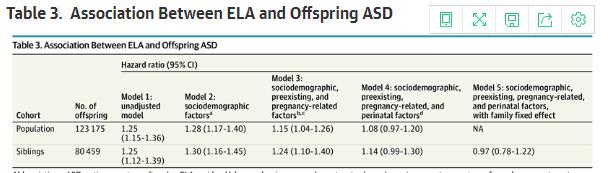
研究包含123175名新生儿数据,其中男孩占50.9%,孕妇生产时的平均年龄为28.2岁,其中47011例(38.2%)新生儿暴露于ELA环境。47011例暴露于ELA的新生儿中有985名(2.1%)确诊为ASD,而76164名未暴露新生儿中1272例(1.7%)确诊(危险比为1.25),但调整母亲社会人口统计学、孕前、妊娠和围产期协变量后,暴露于ELA与后代ASD风险无关(HR=1.08)。在兄弟姐妹亚组中也未发现ELA与ASD有关(HR=0.97)。
研究认为,硬膜外镇痛不会增加后代自闭症谱系障碍风险。
原始出处:
Elizabeth Wall-Wieler et al. Association of Epidural Labor Analgesia With Offspring Risk of Autism Spectrum Disorders. JAMA Pediatr. April 19, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#硬膜外#
29
#DIA#
35
#PE#
20
#自闭症谱系障碍#
49
#镇痛#
35
#自闭#
32
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
38
写的很全面
59
okok
59
好文章
59