Hepatology International:仑伐替尼+TACE对比TACE在不可切除肝癌中的疗效:一项回顾性对照研究
2021-05-10 yd2015 MedSci原创
仑伐替尼+TACE较TACE显著改善不可切除肝癌的临床预后。
肝癌是我国常见的恶性肿瘤。虽然手术是其治愈的手段。但是大部分患者发现时已是不可切除。仑伐替尼目前已被批准用于晚期肝癌一线治疗。经皮动脉化疗栓塞(TACE)在临床上也广泛用于不可切除肝细胞癌(uHCC)患者的治疗中。但是目前没有研究评估两者联合治疗的效果。
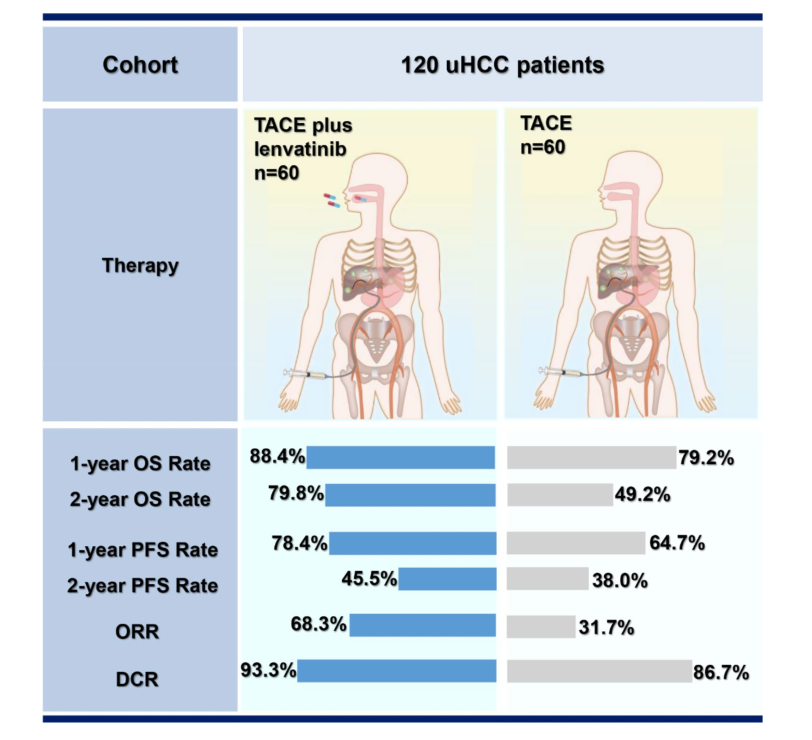
近期,来自上海东方肝胆外科医院的曲增强教授团队,在Hepatology International杂志上发表了一项数据,该研究回顾性分析评估仑伐替尼+TACE对比TACE单独使用在不可切除肝癌中的疗效和安全性。该研究为单中心、回顾性对照研究,主要评估总生存(OS),无进展生存(PFS),客观缓解率(ORR)以及安全性。研究共纳入2017~2019年东方肝胆外科医院治疗的120例不可切除HCC患者,其中仑伐替尼+TACE和TACE组各有60例患者。

研究数据显示,总生存方面,仑伐替尼+TACE组的1年和2年OS率分别为88.4%和79.8%,而TACE单独组则为79.2%和49.2%,HR=0.466 (95%CI: 0.226~0.886, P=0.047)。因此,仑伐替尼+TACE组联合治疗显著延长了患者中位OS。对于无病进展生存方面,仑伐替尼+TACE组的1年和2年PFS率分别为78.4%和45.5%,而TACE单独组则为64.7%和38.0%,HR=0.343(95%CI: 0.198~0.595,p<0.001)。同样联合治疗显著延长了患者PFS。
两组疗效概况

两组OS和PFS
仑伐替尼+TACE组的ORR为 68.3%,而TACE单独组的ORR则为31.7%,有显著统计学意义(P<0.001);两组疾病控制率(DCR)分别为93.3%和86.7%,联合治疗组的DCR数值上也相对更高。
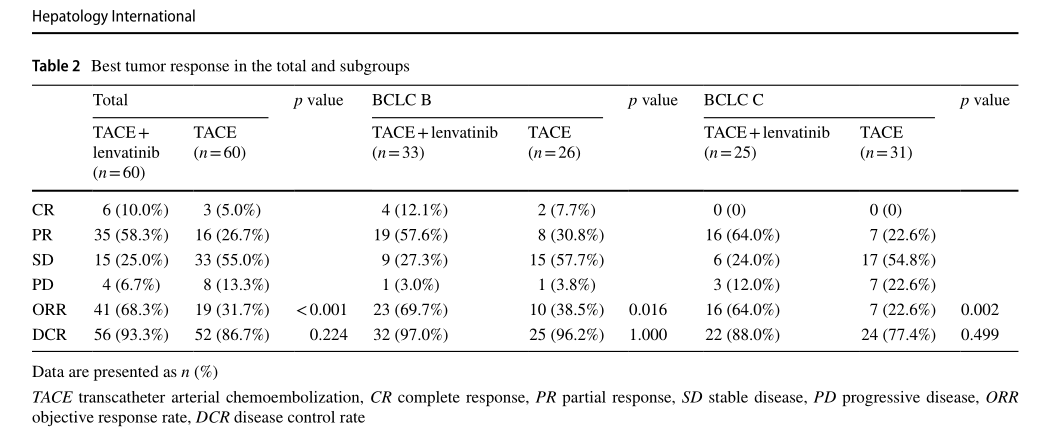
两组的ORR和DCR
从安全性来看,联合治疗组最常见的不良事件为白蛋白减少(55.0% vs. 38.3%)、高血压(48.3% vs. 0)和血小板减少(46.7% vs. 50.0%),最常见的3~4级不良事件为高血压(23.3%),总体上可耐受,可控。
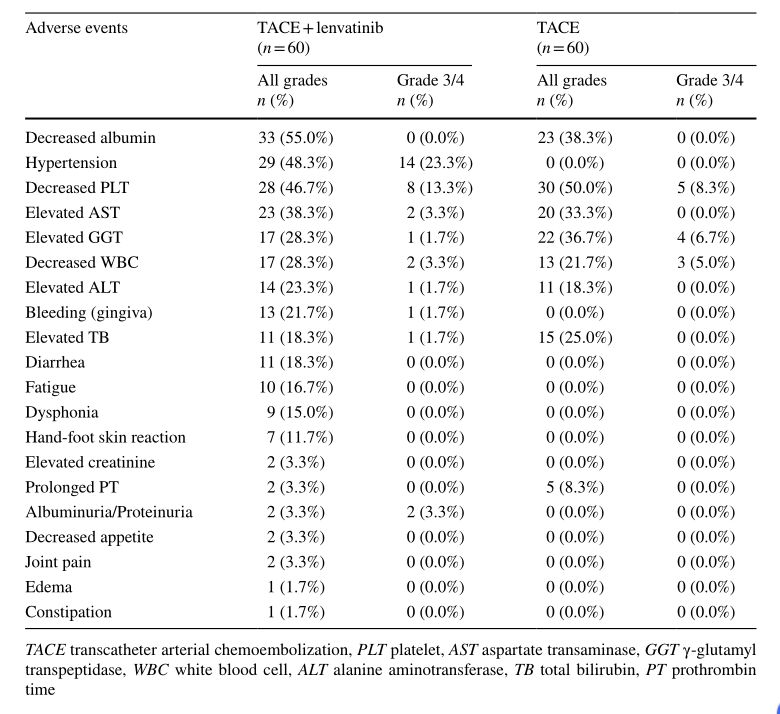
不良事件
综上,仑伐替尼+TACE较TACE单独治疗显著改善不可切除肝癌的临床预后。
原始出处:
Zhigang Fu, Xiaowei Li, Jiaming Zhong, et al. Lenvatinib in combination with transarterial chemoembolization for treatment of unresectable hepatocellular carcinoma (uHCC): a retrospective controlled study. Hepatol Int. 2021 Apr 20. doi: 10.1007/s12072-021-10184-9. Online ahead of print.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TAC#
32
#对照#
27
#ACE#
36
#eRNA#
24
#Nat#
26
#EPA#
25
谢谢梅斯提供这么好的信息,学到很多
37
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
38
好
51
好
50