J Inflamm Res: 多重细胞因子分析:一种早期预测舌下免疫疗法对过敏性鼻炎患者疗效的新方法
2022-03-25 AlexYang MedSci原创
调查AR患者血清中多种细胞因子的水平,并探讨它们与AIT疗效的关系。
过敏性鼻炎(AR)是一种常见的上呼吸道疾病,以IgE介导的Th2炎症为特征。最近,流行病学研究显示,AR影响了全球20%-30%的人口,而且其发病率还在持续上升。目前,避免过敏原、药物治疗和过敏原特异性免疫疗法(AIT)是AR治疗的主要方法,AIT是唯一能够诱导过敏原耐受的疾病调节治疗方法。传统的AIT可以在皮下或舌下进行,而舌下免疫治疗(SLIT)似乎更受欢迎,因为它方便、疗效相当、耐受性好。尽管其在AR患者中的安全性和有效性已被广泛接受,但许多患者仍然反应不佳。因此,探索早期识别反应者的生物标志物或方法,监测被分配到SLIT的AR患者的治疗效果,是一个研究重点,对开发精确的免疫疗法至关重要。
近日,来自西安交通大学第二附属医院的研究人员进行了研究,旨在举例说明AR患者血清中多种细胞因子的水平,并探讨它们与AIT疗效的关系。相关研究结果发表在《Journal of Inflammation Research》期刊上。
研究前瞻性地招募了74名接受舌下免疫疗法(SLIT)治疗的AR患者。研究人员在SLIT开始前采集他们的血清样本,通过多重分析检测细胞因子水平。所有患者均被随访1年以上。研究人员评估了细胞因子水平与SLIT早期疗效之间的关联,并在另一个独立的队列中进一步验证了显著不同的细胞因子。
结果显示,60名患者完成了定期随访。35名患者被归入响应者组,25名患者被归入无响应者组。多重细胞因子分析显示,两组之间的细胞因子水平有显著差异。与无反应组相比,反应组的BAFF和CCL11浓度更高,CCL2、CCL7、IFNγ、IL8、IL10、IL16和IL33的水平更低(P<0.05)。ROC曲线显示,血清BAFF、IFNγ、IL10和IL33水平对SLIT的疗效有强烈的预测作用(曲线下面积<0.7,P<0.05)。在验证队列中,血清IL10和IL33在无反应者中过度表达。响应者组的患者在SLIT后表现出明显较高的IL10水平和较低的IL33(P<0.05),但在无响应者中没有发现统计学差异(P<0.05)。
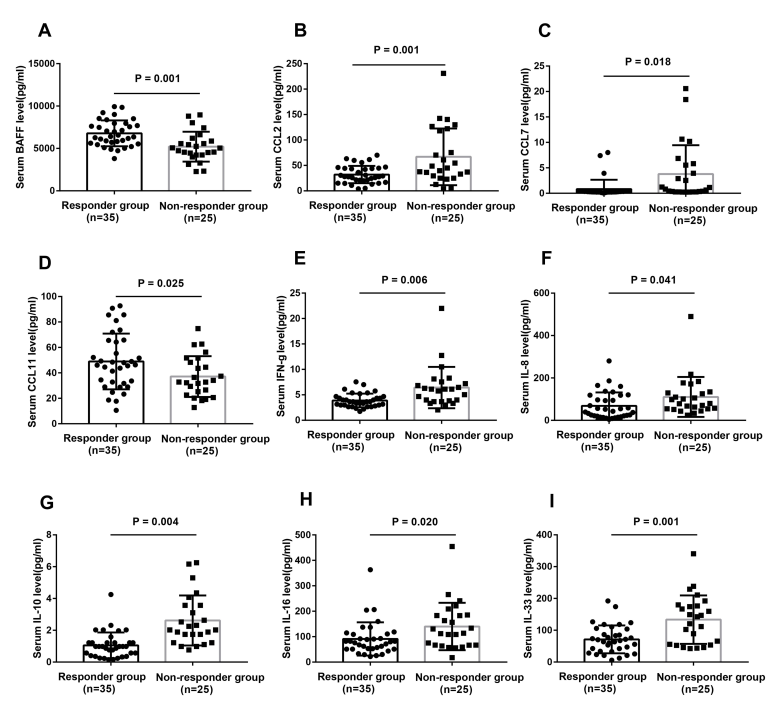
响应者组和无响应者组之间9种不同的细胞因子的血清水平
该研究的数据表明,血清多细胞因子谱与SLIT的反应有关,IL10和IL33或能作为早期预测疗效的新型生物标志物,并参与到AR患者的SLIT治疗机制中。
原始出处:
Yanni Zhang , Kang Zhu , Cui Xia et al. Multiple-Cytokine Profiling: A Novel Method for Early Prediction of the Efficacy of Sublingual Immunotherapy in Allergic Rhinitis Patients. J Inflamm Res. 2022
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#过敏性#
66
#胞因子#
40
#LAM#
36
👍
37
#新方法#
34
#细胞因子#
0
#NFL#
31