Cell Stem Cell:科学家实现人类皮肤细胞向运动神经的定向分化
2017-09-09 海北 MedSci原创
将人类成纤维细胞定向重编程为完全分化的神经元需要进行表观修饰和细胞转录状态的巨大改变。因此,诱导一个特定的染色质环境,使得我们可以得到特定的神经亚型,是细胞命运转化中的主要挑战。
将人类成纤维细胞定向重编程为完全分化的神经元需要进行表观修饰和细胞转录状态的巨大改变。因此,诱导一个特定的染色质环境,使得我们可以得到特定的神经亚型,是细胞命运转化中的主要挑战。
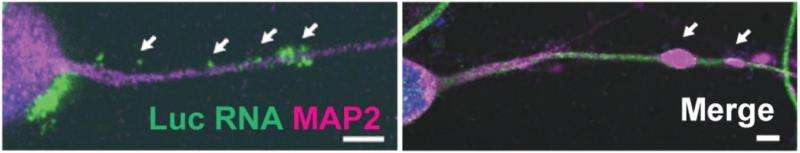
来自华盛顿大学医学院的研究人员证实,脑部富集的miRNA中的miR-9/9 *和miR-124(miR-9/9 * -124)可以引发染色质可及性,DNA甲基化和mRNA表达的重新配置,诱导一个默认的神经元状态。miR-9/9 * -124诱导的神经元(miNs)在功能上是可兴奋的,而且并没有成为特定的神经亚型。但是该细胞在神经元亚型特异性基因处具有开放的染色质状态,表明额外的谱系特异性转录因子可以赋予该细胞特定的亚型身份。研究人员的结果也证实了这一点。他们利用ISL1和LHX3,选择性地将该细胞驱动转化为高度均一的人类脊髓运动神经元。
这项研究表明,miRNA和神经元亚型特异性转录因子之间的协同作用可以推动谱系特异性神经元的重编程,为高效生成不同亚型人类神经元提供了一个通用平台。
原始出处:
Andrew S. Yoo et al. MicroRNAs Induce a Permissive Chromatin Environment that Enables Neuronal Subtype-Specific Reprogramming of Adult Human Fibroblasts. Cell Stem Cell, September 2017 DOI: 10.1016/j.stem.2017.08.002
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Cell#
34
#定向#
27
#CEL#
21
#stem cell#
24
#STEM#
30
#皮肤细胞#
37
好文章.学习了.
72
学习了新知识
76
学习啦!谢谢分享!
70
学习了谢谢分享
53