EJC:心膈角淋巴结与结直肠癌腹膜转移直接相关
2014-02-12 佚名 dxy
腹膜种植转移(PC)的放射学诊断困难重重。在常规实践中,CT检查是是首选的成像方式,然而,它在PC检出中的应用却受到限制。事实上,对于放射学家或训练有素的专家而言,PC诊断中CT扫描的敏感性差别较大,而他们都明了是否应予以检查。每位患者的敏感度值从28%到93%不等,针对每个病灶的敏感度值从9%到100%差别较大,这主要依赖于腹腔种植和局部特征。法国Gustave Roussy 研究院放射科的Ca
法国Gustave Roussy 研究院放射科的Caramella博士等人开展了一项研究,旨在证实心膈角淋巴结是否与结直肠癌腹膜转移有关,论文发布在EJC2014年1月份在线版上。
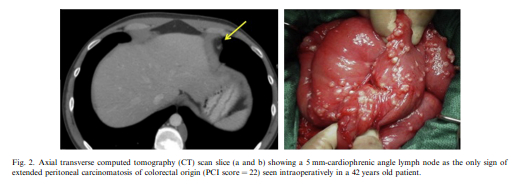
试验中,有550位患者在2007年至2011年间接受过全腹膜手术探查,其中165位患者(30%)当时已经出现了腹膜转移。研究者通过复习患者当时的CT片来查找有无心膈角淋巴结,然后通过单变量和多变量分析来确认结直肠癌腹膜转移与心膈角淋巴结的关系。
结果显示,共有123(75%)例结直肠癌腹膜转移患者发生CPALN,不伴有腹膜转移的结直肠癌患者中有263(68%)人未发现CPALN。经过多变量分析发现,结直肠癌腹膜转移是唯一与CPALN独立相关的因素。CPALN与肝转移无关。研究者观察到,99/165(62%)的腹膜转移的结直肠癌患者在CT片上可以看到明显的标志。剩余的66位患者中的41人,CPALN是结直肠癌腹膜转移的唯一标志。
研究得出如下结论:CT扫描发现心膈角淋巴结(CPALN)或有助于结直肠癌患者发生腹膜转移的诊断。
原始出处
Caramella C, Pottier E, Borget I, Malka D, Goéré D, Boige V, Honoré C, Dartigues P, Dumont F, Ducreux M, Elias D, Dromain C.Value of cardiophrenic angle lymph node for the diagnosis of colorectal peritoneal carcinomatosis.Eur J Cancer. 2013 Dec;
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#淋巴结#
26
#结直肠#
24
#腹膜转移#
27
#腹膜#
28