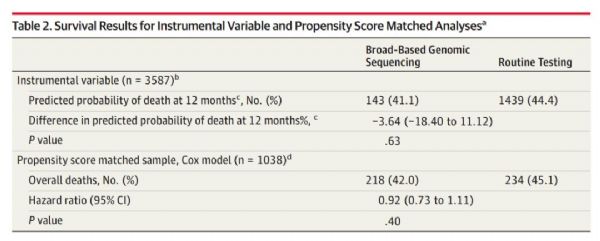
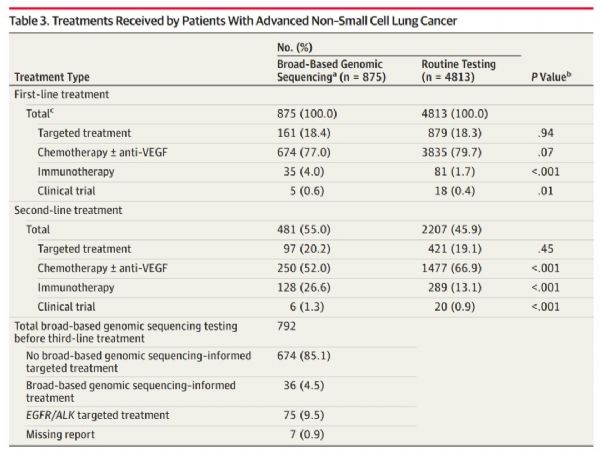
JAMA:测那么多基因也没用?耶鲁科学家发现,广谱基因检测不能提高晚期非小细胞肺癌患者生存率
2018-08-23 奇点糕 奇点网
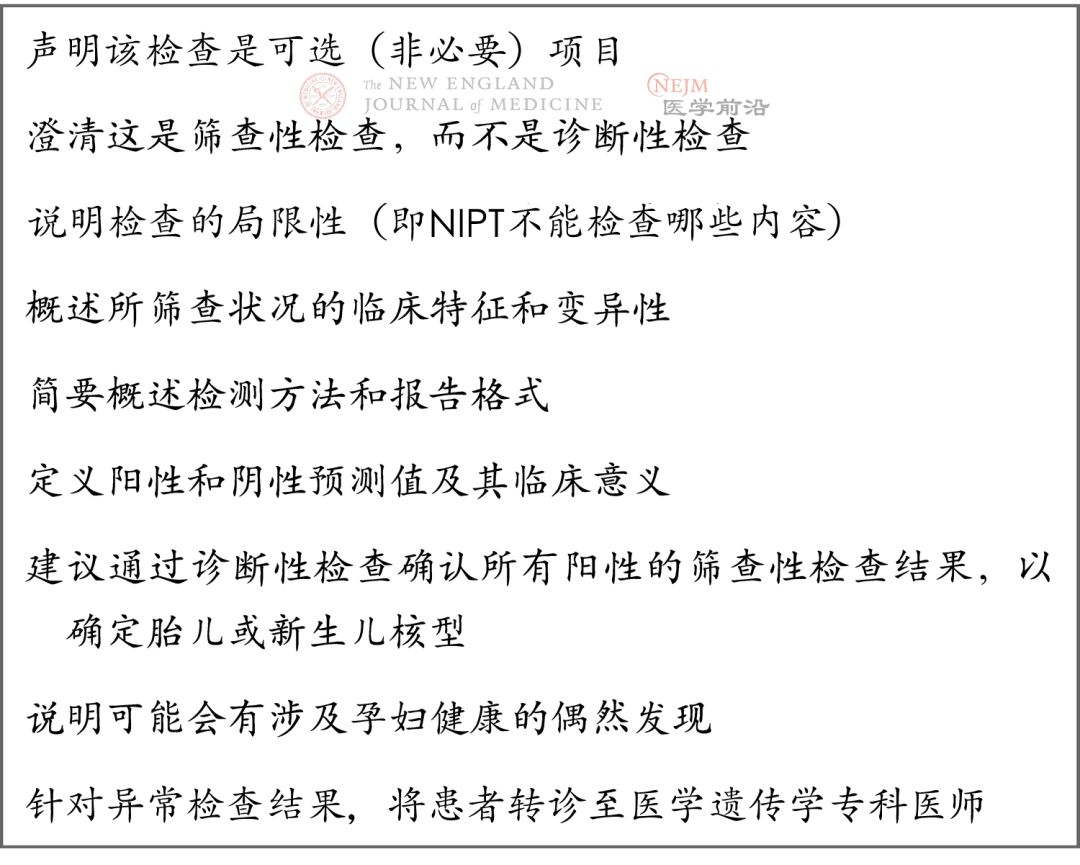
癌细胞大多不止存在一个基因突变,那么同时检测多个基因,也就是我们说的广谱基因检测(BGS),行内人常说的“大panel”,是不是应该给患者带来更好的健康收益呢?
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#科学家发现#
0
#患者生存#
39
#多基因#
33
#非小细胞#
36
#肺癌患者#
21
#生存率#
32
#非小细胞肺癌患者#
30
好
76
了解一下谢谢
65