medRxiv.: 华西领衔的“川军”战队分享COVID-19重症患者的救治经验
2020-04-17 国际循环 国际循环
近日,四川大学华西医院重症医学科康焰团队在预印平台medRxiv发表一项研究论文中,总结了四川省21家重症COVID-19定点医院的临床数据显示,在目前新型冠状病毒肺炎缺乏有效治疗药物的情况下,四川省
近日,四川大学华西医院重症医学科康焰团队在预印平台medRxiv发表一项研究论文中,总结了四川省21家重症COVID-19定点医院的临床数据显示,在目前新型冠状病毒肺炎缺乏有效治疗药物的情况下,四川省的救治经验提示,早期识别并及时给予合理的呼吸支持方式使得重症COVID-19患者的病死率能维持在较低水平。在重症COVID-19病程早期,密切监测与传统氧疗是应该优考虑的救治措施。
SUNRISE研究是一项由四川大学华西医院研究人员发起的多中心队列研究(http://www.chictr.org.cn/index.aspx,ChiCTR2000029758),重点纳入四川省21家COVID-19重症患者制定收治医院的患者数据。在1月16日至3月15日期间,前瞻性或回顾性地收集登记数据。
COVID-19重症患者定义为:1)呼吸困难或呼吸频率≥30/min;2)静息状态下无氧治疗时脉搏血氧饱和度(SPO2)≤93%;3)PaO2:FiO2比值<300;4)24-48小时内肺浸润>50%;5)呼吸衰竭、脓毒性休克和/或多器官功能障碍。
每一位患者从第一天(D1)开始随访,直到出院、死亡或研究结束。第28天(D28)的临床结果包括1)快速恢复(RR):患者D28前完全符合出院标准,体温正常≥3天,呼吸症状和肺部影像学明显改善,呼吸样本两次核酸阴性(采样间隔至少24小时);2)延迟恢复(PR):部分符合D28出院标准,仍需住院治疗,但无晚期呼吸支持;3)未恢复(NR):死亡或D28仍需晚期呼吸支持。
重症COVID-19的早期诊断
使用预先定义的COVID-19重症标准,539例患者中有81例被确定为严重病例。余下的458例非重症COVID19患者中,在研究期间没有观察到死亡。从症状出现到首次住院、RT-PCR确诊和严重疾病诊断的中位时间(IQR)分别为3(1-6)、7(5-10)和9(6-11)天。五项指标中,以PaO2:FiO2比值、SPO2、呼吸困难为多见,分别占87.7%、66.7%和27.2%。在第1天,所有患者(80例CT扫描,1例X线胸片)均显示双肺病变,但仅4例(4.9%)符合影像学诊断标准。患者中位年龄(IQR)为50(39~65)岁,女性占37.0%,BMI≥24kg/m2者占50.6%。43例(53.1%)患者存在慢性共病。Apache II和SOFA评分分别为3(3-5)和10(6-10)。30例(37.7%)患者发生ARDS,6例发生急性肾损伤(AKI),1例符合脓毒性休克标准。患者集中或临时的重症监护治疗
在21家计划中的重症定点医院中,18家在研究期间接受了重症患者治疗。在这些医院中,只有2个有标准的重症监护病房,16个为临时重症监护病房,由传染病综合病房改造而来,配备了重症监护病房的医生和护士。在这种情况下,81例重症患者全部集中到18家定点医院,其中51例(63.0%)在16个临时ICU治疗,30例(37.0%)在2个标准ICU治疗。仅11例(13.6%)直接入院,70例(86.4%)从非定点医院或非危重病例定点医院转院。D1共收治危重病人77例(95.1%)(图1)。
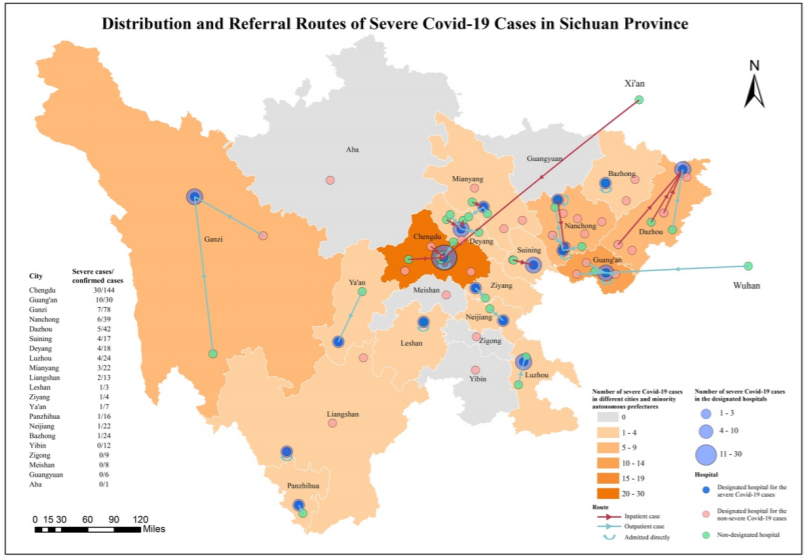 图1. 四川省重症COVID-19的定点医院分布和转诊途径
图1. 四川省重症COVID-19的定点医院分布和转诊途径
呼吸支持是重症COVID-19患者最常用的器官支持方法。在第1天,76例(93.8%)采用呼吸支持,其中51例(67.9%)采用经鼻导管或面罩常规氧疗(COT),13例(16.1%)采用NIV,8例(9.9%)采用HFNC。没有患者插管或需要ECMO。图2显示了从D1到D28给每位患者的每日呼吸支持。在81例确诊为重症的患者中,79例(97.5%)使用COT,31例(38.3%)使用HFNC,22例(27.2%)使用NIV,10例(12.3%)使用IV,1例(1.2%)使用ECMO。34例(81例中42%)仅使用COT,其中79.4%于D28前出院。在25例开始使用COT并需要升级到高级呼吸支持方法的患者中,12例(48.0%)在D28出院。
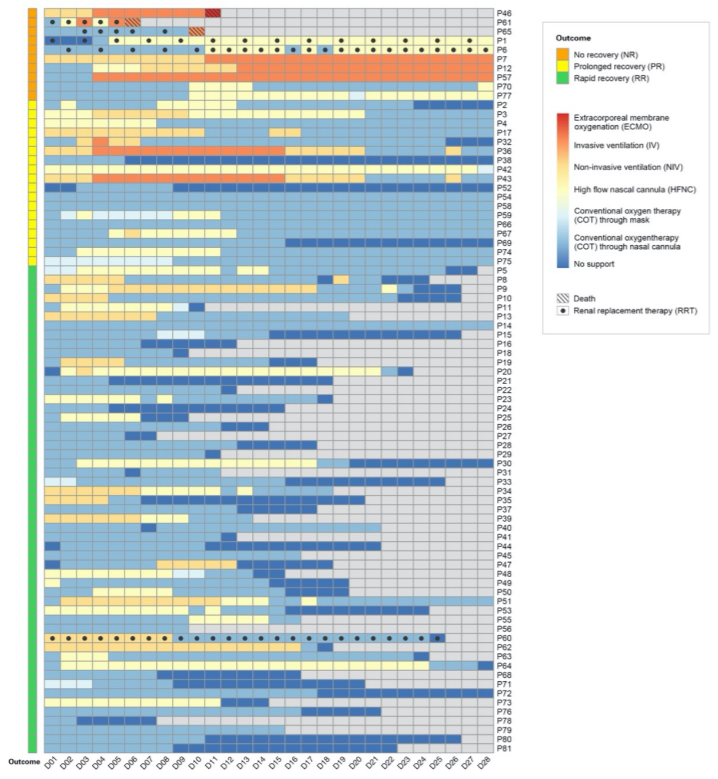
图2. 81例重症COVID-19患者D1~D28的日常器官支持
在28天内出院的患者中,平均住院时间(IQR)为18(14-24)天。只有COT、HFNC和NIV被用作呼吸支持,平均持续时间分别为10(5-14)、0(0-4)和0(0-0)天。对于PR患者,COT、HFNC、NIV和IV分别用于18(7-24)、0(0-7)、0(0-3)和0(0-3)天。对于NR患者,COT、HFNC、NIV和IV的中位持续时间分别为3(1-10)、2.5(0-11)、0(0-3)和2(0-16)天。有1例患者使用ECMO一天。
该研究还分析了呼吸支持的使用情况以及四川新诊断的COVID-19病患者、新诊断的重症患者和住院的重症患者的每日人数(图3)。共使用呼吸支持1579人次/天,其中COT占62.7%(990人次/天),HFNC占19.3%(305人次/天),NIV占9.4%(149人次/天),IV占8.5%(134人次/天),ECMO占0.06%(1人次/天)。呼吸支持高峰持续20天,与危重患者住院需求同步,与四川省初诊患者高峰相比明显滞后9天。在呼吸支持措施最需要的天数内,COT为55.3%,HFNC为21.3%,NIV为12.8%,IV为10.6%。
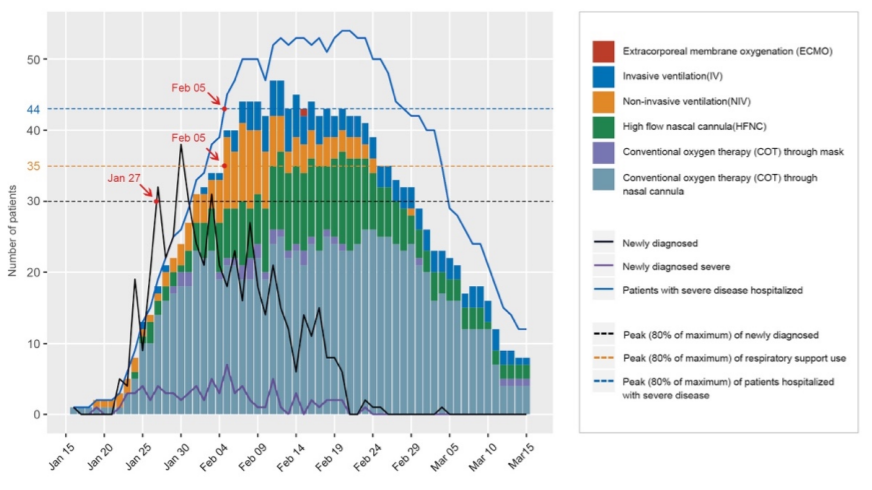
图3.1月16日~3月15日重症COVID-19患者的每日呼吸支持需求
其他支持或医学治疗
部分患者需要采取肾替代(5例,6.2%)、血管加压剂(5例,6.2%)和输血(6例,7.4%)等抢救措施。其他支持方法包括俯卧位、部分肠外营养治疗、止痛药和镇静剂,分别为16例(19.8%)、17例(21.0%)和13例(16.1%)。尽管缺乏有效的循证抗病毒和免疫调节药物,仍给予了各种药物治疗。
患者随访和临床结局
所有患者均随访至研究结束。81例患者中,53例(65.4%)在D28前出院,为快速恢复(RR)。18例(22.2%)为长期恢复(PR),其中13例仍需常规氧疗,5例等待D28的RT-PCR阴性结果。无恢复(NR)共10例(12.3%),其中D28死亡3例,仍需深度呼吸支持7例。3例死者中,1例64岁女性患有硬皮病、肺纤维化和糖尿病,1例80岁女性患有高血压和冠心病。两名患者均出现严重呼吸衰竭并死于多器官功能障碍。第三例患者为73岁男性,患有高血压和终末期肾病,死于循环衰竭。
回顾D1患者的特征可见,NR组患者年龄更大(P<0.001),ApacheⅡ(P=0.01)和SOFA评分更高(P<0.001),合并AKI的可能性更高(P=0.02)(P=0.004)。NR组C反应蛋白(P=0.02)更高,淋巴细胞(p=0.03)和血小板(P=0.005)更低。截至3月15日,仍在D28住院的患者中,15人出院,9人仍在住院,1名81岁男性在D45死于慢性肺疾病。
原始出处:
Xuelian Liao, et al. Critical Care for Severe COVID-19: A Population-based Study from a Province with Low Case-fatality Rate in China. medRxiv. Posted April 05, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










给母校点赞
66
#重症患者#
46
#medRxiv#
62
#华西#
30
#Med#
20