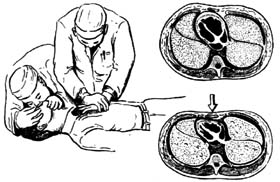
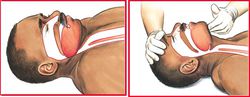
心肺复苏术(cardiopulmonary resuscitation, CPR)过程与图示(图)
2015-12-02 网络 MedSci原创
心搏骤停一旦发生,如得不到即刻及时地抢救复苏,4~6min后会造成患者脑和其他人体重要器官组织的不可逆的损害,因此心搏骤停后的心肺复苏(cardiopulmonary resuscitation, CPR)必须在现场立即进行。基础生命支持(basic life support, BLS)又称初步急救或现场急救,目的是在心脏骤停后,立即以徒手方法争分夺秒地进行复苏抢救,以使心搏骤停病人心、脑及全
心搏骤停一旦发生,如得不到即刻及时地抢救复苏,4~6min后会造成患者脑和其他人体重要器官组织的不可逆的损害,因此心搏骤停后的心肺复苏(cardiopulmonary resuscitation, CPR)必须在现场立即进行。

心肺复苏术
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#IOP#
48
#心肺#
38
#Cardiopulmonary#
28
#resuscitation#
41
#CIT#
35
#心肺复苏术#
35
#ESUS#
27
#pulmonary#
35
#复苏#
25
#CPR#
38