JAMA Neurol:腔隙性梗死静脉溶栓的争论
2019-07-21 杨中华 脑血管病及重症文献导读
阿替普酶静脉溶栓是急性缺血性卒中的有效治疗方案,独立于卒中的亚型。腔隙性梗死的血管病理仍不清楚,腔隙性梗死静脉溶栓的有效性也存在争议。
阿替普酶静脉溶栓是急性缺血性卒中的有效治疗方案,独立于卒中的亚型。腔隙性梗死的血管病理仍不清楚,腔隙性梗死静脉溶栓的有效性也存在争议。远在半个世纪以前,C. Miller Fisher 等的开创性工作发现,腔隙性梗死是由于小穿通动脉闭塞引起的,小穿通动脉闭塞与微小粥样斑(microatheroma)和脂透明变性(lipohyalinosis)有关。血栓在腔隙性梗死病理生理机制中起的作用尚不清楚,因此,有人质疑腔隙性卒中是否能够从溶解血凝块的药物治疗中获益。
另外,严重白质疏松增加静脉溶栓的症状性颅内出血的风险,而腔隙性梗死患者中严重白质疏松很常见。另外,腔隙性卒中的自然史往往更偏良性。这些皆不支持这些患者使用阿替普酶。
卒中溶栓的随机临床试验报道过基于卒中发病机制的亚组结果,包括所谓的腔隙性梗死,但是其诊断依据的是临床表现。然而,这些研究中的腔隙综合征容易与小卒中(根据症状的严重程度)混为一谈。并且,在短时间内腔隙性梗死的诊断需要 MRI 检查(比如,小穿通动脉供血区的皮层下急性缺血病灶),DWI 对诊断急性腔隙性梗死具有很高的敏感性。在以前的溶栓试验中,主要依据平扫 CT,而不是 DWI。
在 WAKE-UP 试验中,所有患者皆进行了 MRI 筛查,DWI 发现急性缺血病灶者才能随机纳入该研究。2019年6月来自德国的Ewgenia Barow等在 JAMA Neurology 上公布了 WAKE-UP 试验的二次事后分析结果,目的在于探讨随机前 MRI 诊断为腔隙性梗死的患者采取静脉溶栓的安全性和有效性。
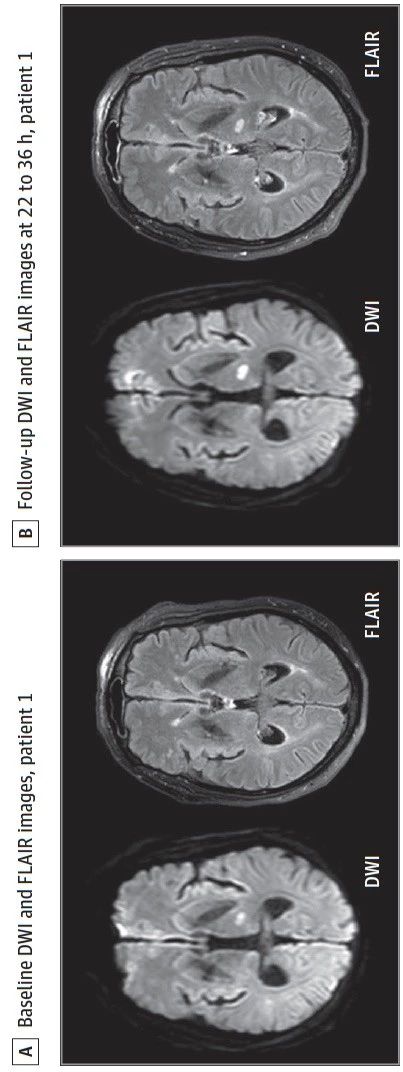
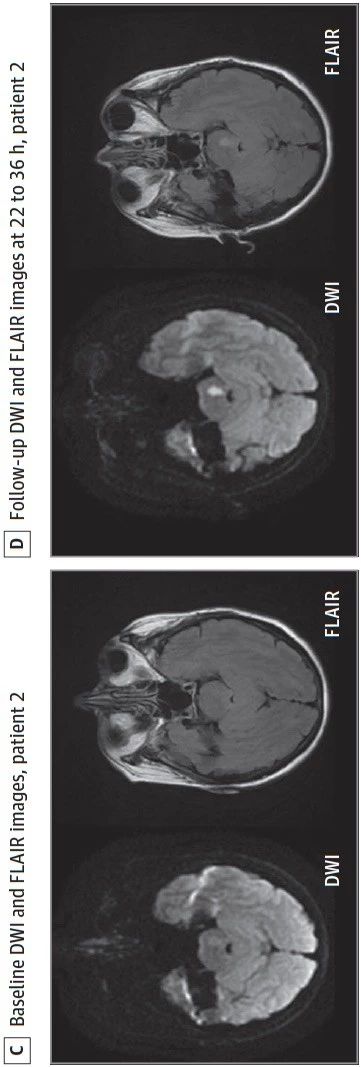
WAKE-UP 是多中心、双盲、安慰剂对照的随机临床试验,纳入的患者为不知道发病时间的急性卒中患者,在 MRI 指导下验证阿替普酶静脉溶栓的有效性和安全性。主要纳入标准为 DWI 发现急性缺血灶,但是相应部位 Flair 未见高信号,这意味着从卒中发作到进行 MRI的时间很可能小于4.5h。该二次事后分析探讨了 MRI 诊断为腔隙性梗死患者采用静脉溶栓的疗效。主要有效性变量为良好预后,定义为90天 mRS 0-1,调整年龄和症状严重程度。
示例:图 A,DWI(+),Flair(-);图 B,DWI(+),Flair(+);图 C,DWI(+),Flair(-);图 D,DWI(+),Flair(+):
在 WAKE-UP 试验中共随机了503例患者,其中108例为影像学诊断的腔隙性梗死,其他395例为非腔隙梗死患者。与非腔隙性梗死相比,腔隙性梗死患者更加年轻(SD,63岁 vs 66岁,P = 0.003)。对于腔隙性梗死的患者,55例设计到阿替普酶组,53例设计到安慰剂组。
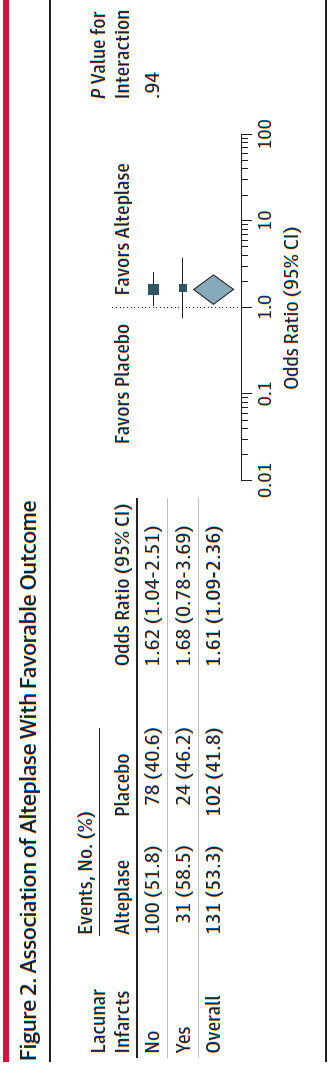
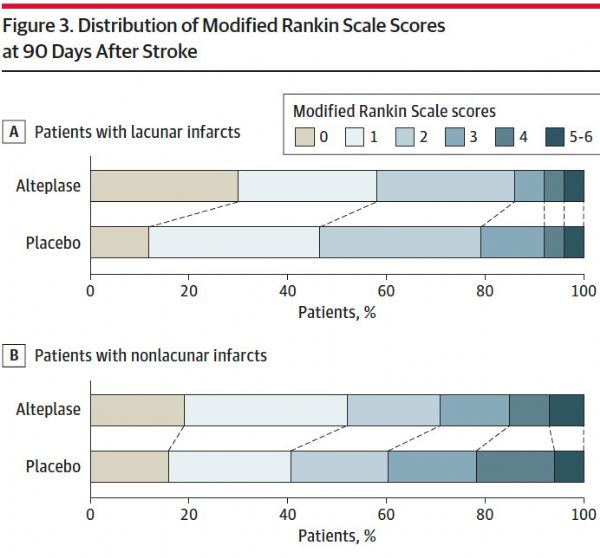
阿替普酶治疗于较高的良好预后比例有关,在腔隙和非腔隙卒中亚型之间,不存在治疗结果的异质性。在腔隙性卒中患者中,阿替普酶组和安慰剂组良好预后的比例分别为59%和46%(adjusted odds ratio [aOR], 1.67 [95%CI, 0.77-3.64])。阿替普酶组1例死亡,1例 sICH;安慰剂组无死亡和sICH。90天 mRS 分布显示阿替普酶治疗有获益的趋势(adjusted common odds ratio of 1.94,95%CI, 0.95-3.93)。
最终作者认为 WAKE-UP 试验二次事后分析的效力不足。这个结果显示对于影像学诊断的腔隙性梗死患者,静脉阿替普酶溶栓和功能预后之间的关系与其他卒中亚型没有显着性差异。
原始出处:Barow E, Boutitie F, Cheng B, et al. Functional Outcome of Intravenous Thrombolysis in Patients With Lacunar Infarcts in the WAKE-UP Trial. JAMA Neurol. 2019 Mar 25.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#Neurol#
21
#静脉#
27
学习了
59
好
59
谢谢了,学习
66