OCC 2017:韩雅玲院士解读2016中国PCI指南
2017-05-26 MedSci MedSci原创
今日,第11届东方心脏病学会议(OCC)开幕式在上海世博中心盛大举行,会议上来自沈阳军区总医院的韩雅玲院士就《中国经皮冠状动脉介入治疗指南(2016)》进行了详细的解读。2016中国PCI指南是在2009和2012年中国PCI指南的基础上编写而成。梅斯小编对韩院士的讲解第一时间做一汇总与大家分享。 新指南的重要更新 优化早期危险评分系统 新指南推荐的早期危险评分系统; 首
第11届东方心脏病学会议(OCC)开幕式在上海世博中心盛大举行,会议上来自沈阳军区总医院的韩雅玲院士就《中国经皮冠状动脉介入治疗指南(2016)》进行了详细的解读。2016中国PCI指南是在2009和2012年中国PCI指南的基础上编写而成。梅斯小编对韩院士的讲解第一时间做一汇总与大家分享。
新指南的重要更新
优化早期危险评分系统
新指南推荐的早期危险评分系统;
首次提出建立质量控制体系,并新增EuroSCORE II和SYNTAX II评分系统;
2012版 IIbB和2016版IIIC的 EuroSCORE评分系统过高地估计了血运重建的死亡风险,新指南通过18项临床特点评估院内死亡率;
SYNTAX评分对于病变既适于PCI又适于CABG且预测外科手术死亡率低的患者,可以继续采用SYNTAX评分帮助制定治疗决策,至今仍在临床广泛使用;
此外,SYNTAX II评分在SYNTAX评分的基础上新增是否存在无保护左主干病变,并联合了6项临床因素,在预测左主干和复杂三支病变血运重建的远期死亡率方面,优于单纯的SYNTAX评分。
血运重建更加强调证据并注重实用
SCAD:优化患者血运重建的推荐,低中危患者PCI推荐级别升高
新指南建议以冠脉病变直径狭窄程度作为是否敢于的决策依据,狭窄≥90%时,可直接干预;狭窄<90%时,应对有缺血证据,或FFR≤0.8的病变进行干预;
重建推荐:针对预后,两支或三支冠状动脉直径狭窄>70%且左心室功能受损(LVEF<40%),单一开放冠状动脉直径狭窄>50%;
针对症状,任一冠状动脉直径狭窄>70%,表现为活动诱发的心绞痛或等同症状,并对药物治疗反应欠佳。
针对合并左主干和/或前降支近端病变,多支血管病变患者,选择合适的血运重建策略。
NSTE-ACS:对极高危患者2h内紧急造影推荐级别升高
对于血流动力学不稳定或心源性休克、顽固性心绞痛、危及生命的心律失常或心脏骤停、心肌梗死机械性并发症、急性心力衰竭伴难治性心绞痛和ST段改变、再发心电图ST-T动态演变,尤其是伴有间歇性ST段抬高的患者,均推荐进行紧急冠状动脉造影(<2h);
对于肌钙蛋白升高、心电图ST段或T薄动态演变(有或无症状)、GRACE评分>140分,推荐早期侵入策略(<24h);
对于中危患者推荐侵入策略(<72h)。
STEMI:推荐无法及时性PCI时在30min内尽早启动溶栓,成功溶栓后行常规PCI,补救性PCI推荐级别增加
如预计FMC至PCI的时间延迟>120min,对有适应症的患者,应于30min内尽早启动溶栓治疗(I,A);
建议溶栓成功24h内行冠状动脉造影并根据需要对IRA行血运重建,溶栓后出现心源性休克或急性严重心力衰竭时建议行急诊冠脉造影并对IRA行血运重建;
对建议溶栓失败者行急诊补救性PCI的推荐级别升高。
STEMI:推荐多支病变STEMI患者开通非梗死动脉
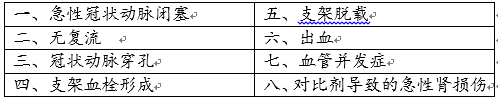
新增PCI术中操作和并发症处理的推荐
手术入路:优选桡动脉路径
尽管股动脉径路是PCI的经典径路,但随着技术的发作,目前在我国大多选择经桡动脉径路(血管相关并发症少、患者痛苦少),应作为首选推荐(I,A);
特殊情况下可酌情选择其他适应的血管径路,如尺动脉、肱动脉等。
辅助技术:强调辅助诊断和治疗技术的重要性,推荐运用IVUS、FFR或OCT帮助决策
IVUS有助于查明支架失败原因,对于选择性患者(无保护左主干、三支分叉、CTO病变及支架内再狭窄病变等)推荐IVUS指导的优化支架置入;
对于没有缺血证据的SCAD患者,推荐对冠脉造影目测直径狭窄50%-90%的病变行FFR评估;对于多支血管病变患者,推荐FFR指导的PCI;
OCT对于诊断血栓、造影未识别的斑块破裂及支架膨胀不良的价值优于IVUS;
支架选择:高再发缺血风险者应优选新一代DES
左主干合并分叉病变和CTO病变,优先考虑应用新一代DES,以降低再狭窄率
PCI主要8个并发症防治措施
抗栓治疗: ACS患者抗血小板治疗优选替格瑞洛;抗凝治疗比伐卢定推荐级别上升
NSTE-ACS:推荐优选替格瑞洛;STEMI:尽早给予P2Y12受体抑制剂
ACS:比伐卢定证据水平增加
NSTE-ACS: PCI术中使用比伐卢定(一次性静脉注射0.75mg/kg,随后1.75 mg/kg /h维持至术后4h)作为普通肝素合用GPI的替代治疗;
STEMI:PCI术中使用比伐卢定(一次性静脉注射0.75mg/kg,随后1.75 mg/kg /h维持至术后4h)。
我国BRIGHT研究:与肝素或肝素+替罗非班相比,单用比伐卢定显著降低30天净临床事件发生风险
8种特殊风险人群抗栓治疗
1. 糖尿病患者:抗血小板治疗首选替格瑞洛
2. CKD患者:首选替格瑞洛,且无需调整剂量;在接受透析治疗的患者中使用替格瑞洛经验较少,可选择氯吡格雷
3. 复杂冠脉病变患者:首选替格瑞洛
4. 非心脏外科手术患者:抗血小板方案的调整应充分权衡外科手术的紧急程度和患者出血及血栓风险,对心脏事件低危患者,术前5-7天停用DAPT,术后保证充分止血可重新用药
5. CYP2C19慢代谢及血小板高反应性者:如无出血高危因素,应优先选择替格瑞洛
6. 对CHA2DS2-VAS评分≥2分、HAS-BLED≤2分的SCAD合并心房颤动患者:建议置入BMS或新一代DES后口服抗凝药物+阿司匹林100mg/d、氯吡格雷75 mg/d至少一个月,然后口服抗凝药+阿司匹林100mg/d或氯吡格雷75 mg/d维持至少1年
7. 对ACS合并心房颤动者:如HAS-BLED评分≥2分,建议不考虑支架类型,均口服抗凝药+阿司匹林100mg/d、氯吡格雷75 mg/d六个月,然后口服抗凝药+阿司匹林100mg/d或氯吡格雷75 mg/d维持至少1年
8. HAS-BLED评分≥3分需口服抗凝药的冠心病患者(SCAD和ACS):建议不考虑支架类型,口服抗凝药+阿司匹林100mg/d、氯吡格雷75 mg/d至少一个月,然后口服抗凝药+阿司匹林100mg/d或氯吡格雷75 mg/d(持续时间根据临床具体情况而定)
细化PCI术后管理及随访内容
围术期及术后管理:细化术后管理及随访内容
1. 对于某些特定患者(合并糖尿病;未完全血运重建等)建议早期复查冠脉造影或CTA
2. PCI术后>2年患者应常规行负荷试验
3. 负荷试验提示中高危的患者应付差冠脉造影
4. 高危患者PCI后无论有无症状,术后3~12个月复查冠脉造影
5. 康复治疗,ACS患者PCI治疗后应实施以合理运动为主的心脏康复治疗
6. 对冠心病患者,无论何种类型,均推荐长期服用他汀类药物,使用LDL-C<1.8mmol/L
7. 亚洲与我国的研究结果显示,PCI术前使用负荷剂量他汀不优于常规剂量,不建议对ACS患者PCI术前使用负荷剂量他汀
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#韩雅玲院士#
27
学习了谢谢分享!!
67
#OCC#
22
#韩雅玲#
45
学习了谢谢分享。
65
学习了,提高了
49
学习了,不错
62
学习了,指南要分享。
61