脾硬化性血管瘤样结节性转化超声造影1例
2019-04-09 李丽 薛红元 聂晓彤 中国超声医学杂志
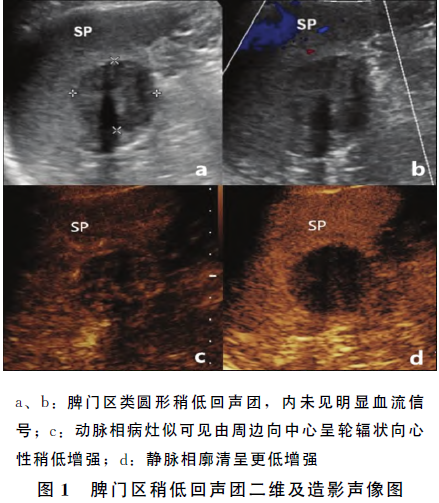
患者女,71岁。因“查上腹部CT平扫发现脾脏实质内低密度影”,于2017年10月26日入院。体格检查:腹软,无肠型及蠕动波,左上腹轻度压痛,轻度肌紧张,无叩击痛及反跳痛,肝脾肋下未触及。超声检查:于脾门区可探及一大小约32.9mm×345mm×36.1mm的类圆形稍低回声团,与脾分界不清,病灶内可见声影;CDFI:病灶内未见明显血流信号。
患者女,71岁。因“查上腹部CT平扫发现脾脏实质内低密度影”,于2017年10月26日入院。体格检查:腹软,无肠型及蠕动波,左上腹轻度压痛,轻度肌紧张,无叩击痛及反跳痛,肝脾肋下未触及。超声检查:于脾门区可探及一大小约32.9mm×345mm×36.1mm的类圆形稍低回声团,与脾分界不清,病灶内可见声影;CDFI:病灶内未见明显血流信号。
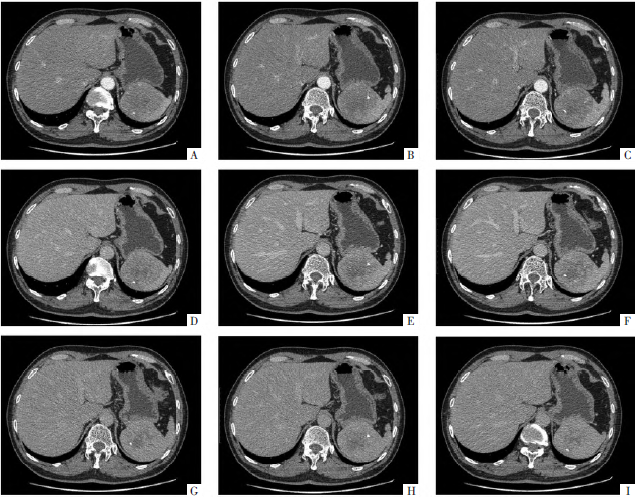
超声造影检查:动脉相病灶似可见由周边向中心呈轮辐状向心性稍低增强,静脉相廓清呈更低增强;超声造影提示:脾门区乏血供占位,考虑良性病变。CT平扫+增强:脾内侧类圆形稍低密度影,增强扫描呈渐进性强化,性质待定。同年11月2曰患者在本院行腹腔镜下脾切除术。病理诊断:脾硬化性血管瘤样结节性转化。
讨论
脾硬化性血管瘤样结节性转化(scleroring angiomatoid nodular transformation,SANT)是一种极为罕见的良性血管瘤样疾病。病因尚不清楚,有人提出SANT可能与全身炎症反应和EB病毒感染有关,也有学者认为SANT可能是继发于循环障碍或创伤引起的组织血肿,进而结节性转化。多数患者无明显症状,仅在体检时偶然发现脾脏占位性病变,少数患者可因触及脾脏肿块或腹部疼痛不适而就诊。在二维超声检查中,SANT通常表现为不均匀低回声团块伴有线样回声,病灶中央多有声影。
超声造影一般表现为动脉相早期出现由外周向中心的轮辐状增强;静脉相与脾实质相比,病灶呈稍低增强。这种类似于肝脏局灶性结节性增生的增强模式,被认为是脾脏SANT的特征表现。其病理基础为,肿瘤大体切面可见致密的纤维组织及由外向内延伸的动脉分支,呈血管瘤样结节表现。本例患者的二维及超声造影的声像图特征与文献报道基本相符,符合SANT的超声表现(图1)。
综上所述,在影像学检查发现脾脏有孤立性病变时,应当考虑到SANT的可能。超声造影检查具有比增强CT更好的时间分辨率,并且可以动态地显现病灶的血流分布情况。因此,超声造影可对脾脏SANT的诊断提供重要线索。
原始出处:
李丽,薛红元,聂晓彤.脾硬化性血管瘤样结节性转化超声造影1例[J].中国超声医学杂志,2018(02):192.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#脾硬化性#
44
#超声造影#
47
#结节性#
32
#血管瘤#
39
#造影#
45
#硬化性#
28
好
54