Dig Dis:不经活检确认的放大内镜联合蓝激光成像对胃部肿瘤分界诊断的有效性和可行性
2021-07-25 MedSci原创 MedSci原创
准确诊断胃肿瘤的分界线(DL)对于通过内窥镜粘膜下剥离术(ESD)进行瘤体完切至关重要。在ESD之前,只进内镜诊断胃肿瘤的DL是有争议的。近日,一项前瞻性的单中心研究评估了仅使用放大内镜联合蓝激光成像
准确诊断胃肿瘤的分界线(DL)对于通过内窥镜粘膜下剥离术(ESD)进行瘤体完切至关重要。在ESD之前,只进内镜诊断胃肿瘤的DL是有争议的。近日,一项前瞻性的单中心研究评估了仅使用放大内镜联合蓝激光成像(M-BLI)与同时使用M-BLI和活检确认对胃腺瘤和分化良好的腺癌的DL的诊断准确性,研究结果已发表于Dig Dis。
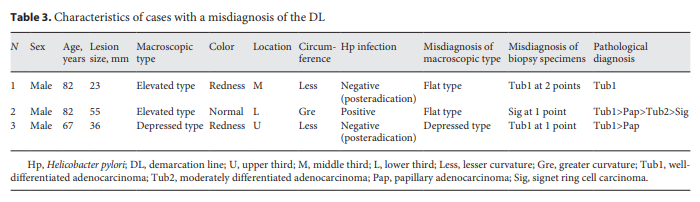
2015年7月至2016年12月期间,研究纳入了96个分化良好的腺癌和32个胃腺瘤。共有122个在M-BLI上有明确DL的病变被随机分配到仅接受M-BLI(M-BLI组)或M-BLI与活检确认(M-BLI-BC组),在ESD前从病变外≈5毫米的非癌组织的4个方向进行活检。主要目的是确定在诊断准确性和完全切除方面,没有活检确认的M-BLI与有活检确认的M-BLI相比是否有劣势。
结果显示,两组之间在性别、中位年龄、肤色、周长、大体类型、基于活检的诊断和幽门螺杆菌感染方面没有显著差异。M-BLI和M-BLI-BC组的DL诊断准确率分别为100和95.0%,完全切除率均为100%。
综上,该研究结果表明,M-BLI的诊断能力在诊断胃腺瘤和分化良好的腺癌的分界方面非常好。对于这些病变,通过M-BLI明确的DL,不需要进行活检确认。
原始出处:
Takahiro Nakano, et al., Efficacy and Feasibility of Magnifying Blue Laser Imaging without Biopsy Confirmation for the Diagnosis of the Demarcation of Gastric Tumors: A Randomized Controlled Study. Dig Dis. 2021;39(2):156-164. doi: 10.1159/000510559.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Dis#
22
#可行性#
43
#内镜#
26
#活检#
27
#激光#
18
学到了,谢谢
52