Alz Res Therapy:简易认知量表测试,或可辅助筛查阿尔兹海默症病理筛查
2021-11-08 Freeman MedSci原创
BHA措施与Aβ和区域tau的体内成像标志物明显相关,可用于识别临床实践中疑似AD病理的患者
一些研究已经调查了认知措施和AD PET病理标志物之间的关系。具体来说,过去的研究发现tau-PET和认知之间有中度到强度的关联,表明tau示踪剂结合的地形与典型和非典型AD相关领域的认知表现相吻合。此外,tau-PET与认知正常的老年人的认知表现和衰退有关,也与混合临床样本的功能损害的严重程度有关。

同样,Aβ-PET负担和认知之间的关系在临床混合样本和认知无障碍样本中都有报道,包括认知正常的Aβ阳性(Aβ+)老年人的下降率更高。
然而,与tau相比,更大的Aβ负担对认知表现的影响往往更弱,这可能是由于tau病理与受影响脑区的神经元损失关系更密切。同时,PET研究在很大程度上仍然是成本高昂,无法广泛使用,仍然需要简短和高效的工具来检测AD病理。考虑到体内标志物与认知的关联,简短、可靠和敏感的认知措施有可能作为一线成本效益的临床标志物满足这一需求。
与Aβ和tau标志物密切相关的及时和具有成本效益的临床标志物可能有助于大大减少临床上对PET扫描的需求,并实现多模式的病例识别,作为漫长的临床和诊断评估的一个可扩展的替代方案。这些非侵入性的一线措施不会取代全面的临床和神经心理学评估以及标准的成像和实验室测试,而是通过为提供者提供一种手段来确定谁需要转诊进行综合评估以进行诊断确认,从而提高这些诊断研究的临床效率。此外,对认知功能的强大的多领域测量将加强PET结果对临床影响和护理路径的实施,特别是考虑到过去对认知无障碍的人的PET阳性结果的证据。
藉此,UCSF的Elena Tsoy等人探讨了加州大学旧金山分校(UCSF)脑健康评估(BHA)的认知表现之间的关联,这是一个基于平板电脑的简短量表,开发并验证了用于检测老年人的神经认知障碍。
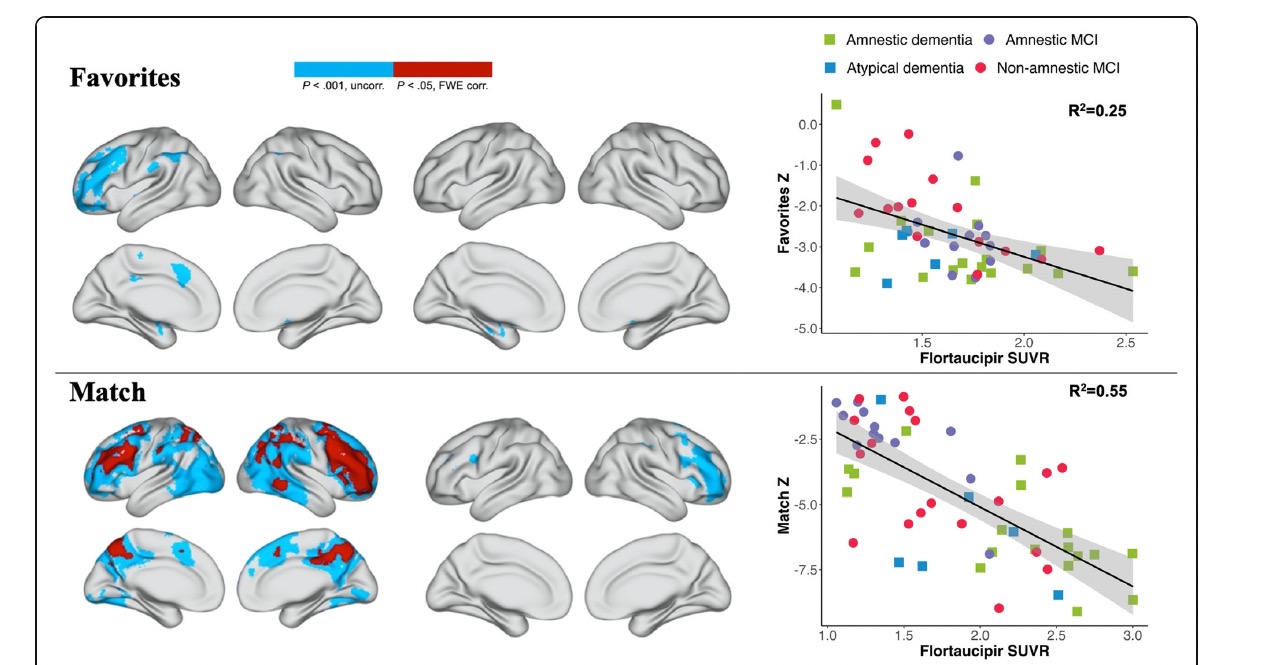
他们在轻度认知障碍(MCI)或痴呆症患者(N = 140;43 Aβ-,97 Aβ+)中使用逻辑回归模型研究了基于脑健康评估(BHA)片剂的认知测量与二分法Aβ-PET状态的关系。我们还在60名Aβ+的MCI或痴呆患者的子样本中使用体素明智回归分析,调查了BHA测试和tau-PET信号的区域模式之间的关系。
他们发现:Favorites(联想记忆)、Match(执行功能和速度)和日常认知量表得分与Aβ阳性显著相关(曲线下面积[AUC] = 0.75 [95% CI 0.66-0.85])。
在MCI和痴呆症患者的子样本中,中颞区的Favorites、额顶区的Match和枕顶区的Line Orientation(视觉空间技能)与Tau-PET信号有明显的关联。
这个研究的重要意义在于发现了:BHA措施与Aβ和区域tau的体内成像标志物明显相关,可用于识别临床实践中疑似AD病理的患者。
原文出处:
Tsoy E, Strom A, Iaccarino L, et al. Detecting Alzheimer’s disease biomarkers with a brief tablet-based cognitive battery: sensitivity to Aβ and tau PET. Alz Res Therapy. 2021;13(1):36. doi:10.1186/s13195-021-00776-w
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言





















#ERA#
29
#阿尔兹海默#
38
学习了
61
学习了
69
坚持学习
60