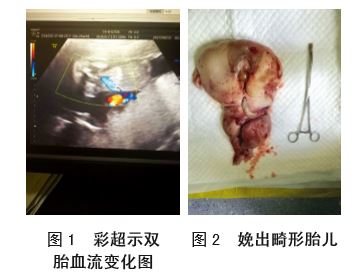
双胎无心无脑畸形不良结局报道一例
2019-06-11 罗梦瑶 徐淑波 王合 中国妇产科临床杂志
患者44岁,孕31+4 周,孕4产2,孕早期无不良接触 史,未行规范产检及产前诊断。孕11周检查发现“2型糖 尿病”,空腹血糖波动于11.2~14.1 mmol/L,餐前及餐后血 糖均大于20 mmol/L,胰岛素治疗后,空腹血糖控制在6~ 7 mmol/L,餐后2 h血糖控制于11~12 mmol/L。孕24周首次 行彩超提示“双胎其一为双胎反向动脉灌注序列征(无头无 心畸形)、胎儿水肿(淋巴水
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












了解一下
56
了解一下
62
了解一下
76
了解一下
56
#畸形#
21