基于测量的协议提高了儿童超声心动图评估肺动脉高压-右心室收缩压的评估者间一致性和准确性
2022-07-19 刘少飞 MedSci原创
评估了实施基于测量的协议对 IR 协议和儿童右心室 (RV) 收缩压报告准确性的影响。
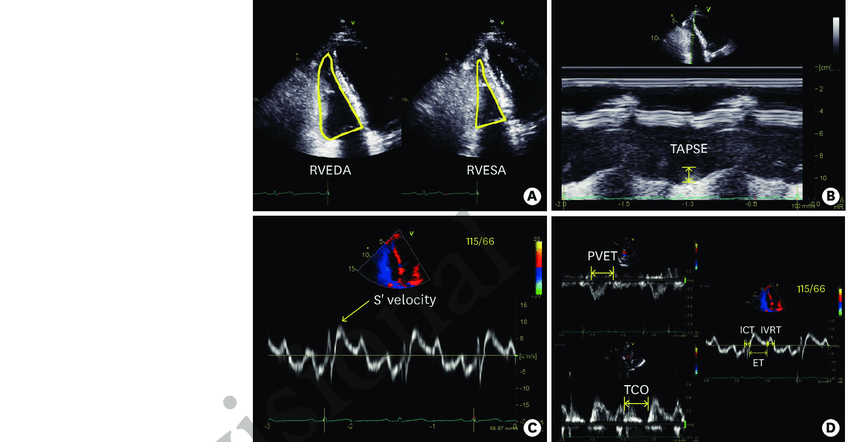
近年来,随着超声技术的不断发展,三维超声心动图和心肌应变显像技术在心功能检查中的应用,使我们对于心功能的超声测量方法有了新的认识。超声心动图测量有望改善主观评估的评分者间一致性 (IR)。在这项研究中,我们评估了实施基于测量的协议对 IR 协议和儿童右心室 (RV) 收缩压报告准确性的影响。我们还评估了该报告协议对 IR 协议在报告 RV 扩张、肥大和收缩功能方面的影响。
研究方法:
五位超声心动图阅读者报告了他们对 40 个未识别超声心动图的 RV 收缩压、扩张、肥大和收缩功能的评估,他们使用各自的习惯方法,然后使用仅基于 RV 测量的商定方案。使用 kappa 统计评估 IR 协议。与通过心导管术获得的血流动力学数据相比,使用 McNemar 测试评估了 RV 收缩压等级的准确性。使用组内相关系数 (ICC) 和变异系数 (CoV) 评估 RV 测量的可靠性。
研究结果:
使用基于测量的协议后,IR 一致性和 RV 收缩压评估的准确性得到改善 [一致性:0.39(95% 置信区间:0.27,0.5)至 0.62(0.48,0.76)和准确性 18/40 至 29/40 p = 0.03]。RV 扩张的 IR 一致性提高 [0.36 (0.25,0.48) 至 0.63 (0.48,0.79)],而 RV 肥大 [0.29 (0.17,0.42) 至 0.35 (0.15,0.55)] 和 RV 收缩功能 [0.57 ( 0.45,0.69) 到 0.53 (0.41,0.66)] 没有改善。测量的可靠性很好 (ICC > 0.8),除了 RV 游离壁厚度 (ICC: 0.62, CoV: 24%) 和 RV 部分面积变化 (ICC: 0.47, CoV: 22%) 提出了缺乏的可能原因改善右室肥大和右室收缩功能的 IR 一致性。
研究结论:
使用 RV 测量代替主观评估的报告协议标准化提高了 IR 一致性和 RV 收缩压评估的准确性。可靠的测量结果,RV 收缩压和扩张,导致 IR 一致性的改善,而不可靠的测量结果,RV 肥大和收缩功能则没有。在设计临床方案以减少作为错误来源的 IR 分歧时,需要特别注意测量的可靠性和可靠性的异方差性。
参考文献:
Nawaytou H, Springston C, Lazar A, Keller S, Hogan W, Cresalia N, Peyvandi S, Cocalis M, Moon-Grady A, Brook M. A Measurement-Based Protocol Improves Inter-Rater Agreement And Accuracy of Right Ventricular Systolic Pressure Assessment by Echocardiography in Children: A Call for Quality Improvement. J Am Soc Echocardiogr. 2022 Jul 12:S0894-7317(22)00346-7. doi: 10.1016/j.echo.2022.06.014. Epub ahead of print. PMID: 35840083.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#一致性#
31
#动脉高压#
50
#收缩压#
42
#心动图#
50
#准确性#
34
#右心室#
44