Clin Cancer Res:MEDI0680联合杜瓦鲁单抗治疗晚期肾透明细胞癌
2022-06-16 MedSci原创 MedSci原创
MEDI0680联合杜瓦鲁单抗在晚期透明细胞癌患者中的安全性和耐受性良好,但是与纳武单抗单药治疗相比,不能提高疗效
MEDI0680是一种人源抗PD-1抗体,杜瓦鲁单抗(Durvalumab)是一种抗PD-L1抗体。与单纯阻断PD-1相比,抗PD-1抗体和抗PD-L1抗体联合使用或可增强疗效。
该研究是一项开放标签的随机II期临床试验,评估了MEDI0680联合杜瓦鲁单抗相比纳武单抗单药治疗在免疫疗法初治的晚期肾透明细胞癌中的抗肿瘤活性和安全性。
既往至少进行过一次抗血管生成治疗的晚期肾透明细胞癌患者随机接受MEDI0680(20 mg/kg)+杜瓦鲁单抗(750 mg)或纳武单抗(240 mg)治疗,两周一疗程。主要终点是客观缓解率(ORR)。次要终点包括最佳缓解率、无进展生存期(PFS)、安全性、总生存期(OS)和免疫原性。探索性终点包括循环肿瘤DNA(ctDNA)的变化、基线肿瘤突变负荷和肿瘤浸润免疫细胞谱。
两组患者的治疗反应
共有63位患者被随机分至联合组(n=42)或纳武单抗组(n=21)。联合组和纳武单抗组的客观缓解率分别是16.7%和23.8%。两组的中位无进展生存期均是3.6个月,中位总生存期都未达到。因不良反应,23.8%的患者停用MEDI0680和杜瓦鲁单抗,14.3%的患者停用纳武单抗。
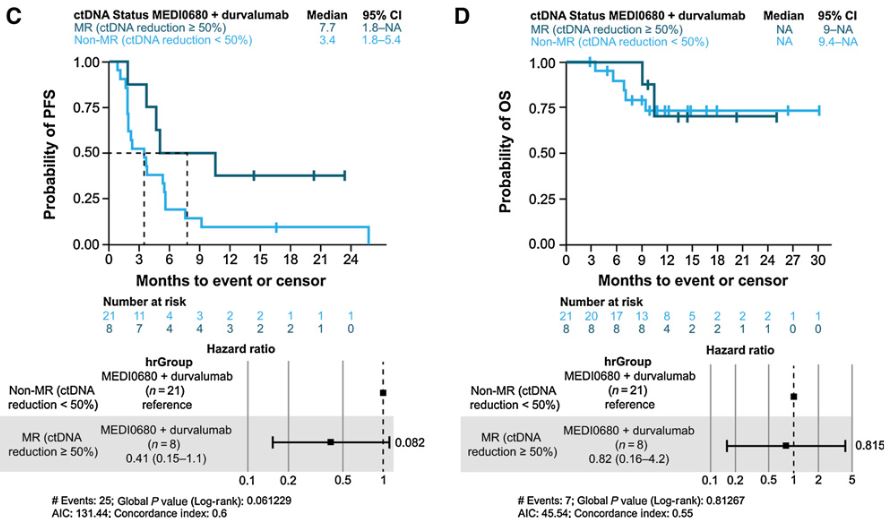
联合组ctDNA降低50%与否患者的PFS率和OS率
在联合组,ctDNA比例降低与更长的PFS相关。ctDNA突变分析未发现与任何一组的治疗反应相关。肿瘤浸润免疫细胞谱显示免疫细胞激活和联合组的治疗反应相关。
综上,MEDI0680联合杜瓦鲁单抗在晚期透明细胞癌患者中的安全性和耐受性良好,但是与纳武单抗单药治疗相比,该联合方案并不能提高疗效。
原始出处:
Martin H. Voss, Arun A. Azad, Aaron R. Hansen, et al. A Randomized Phase II Study of MEDI0680 in Combination with Durvalumab versus Nivolumab Monotherapy in Patients with Advanced or Metastatic Clear-cell Renal Cell Carcinoma. Clin Cancer Res 2022; https://doi.org/10.1158/1078-0432.CCR-21-4115.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#细胞癌#
46
#透明细胞癌#
43
#Med#
40