经皮内窥镜下腰椎间盘切除术后并发假性囊肿3例
2019-08-06 吴环宇 张明彦 刘向阳 中国脊柱脊髓杂志
病例1,女性,33岁,因“反复腰部疼痛7年,再发伴左下肢疼痛20d”入院。查体:左侧大腿后方S1根性痛;影像学检查:腰椎CT、MRI示L5/S1椎间盘向左后方脱垂压迫左侧S1神经根(图1)。诊断:腰椎间盘突出症(L5/S1)。于2015年7月19日硬膜外麻醉下行椎板间隙入路脊柱内镜髓核摘除+纤维环汽化成形术,术后症状即刻缓解。复查CT,矢状位示脱垂髓核已摘除,横断位仍可见疑似椎间盘突出征象,其实为
临床资料
病例1,女性,33岁,因“反复腰部疼痛7年,再发伴左下肢疼痛20d”入院。查体:左侧大腿后方S1根性痛;影像学检查:腰椎CT、MRI示L5/S1椎间盘向左后方脱垂压迫左侧S1神经根(图1)。诊断:腰椎间盘突出症(L5/S1)。于2015年7月19日硬膜外麻醉下行椎板间隙入路脊柱内镜髓核摘除+纤维环汽化成形术,术后症状即刻缓解。复查CT,矢状位示脱垂髓核已摘除,横断位仍可见疑似椎间盘突出征象,其实为内镜术后术区水肿信号(图2)。术后1个月,患者出现下腰部酸胀疼痛及左下肢大腿后侧放射性疼痛。门诊复查MRI示原手术节段出现T2加权像高信号,T1加权像低信号类圆形影,10×6mm,压迫左侧S1神经根(图3),予以卧床休息、口服非甾体类消炎止痛药物2周后,门诊随访,患者症状缓解。

病例2,男性,20岁,因“反复腰背部伴右下肢疼痛6个月,加重1个月”入院。查体:右下肢L5根性痛。影像学:腰椎CT、MRI示L4/5椎间盘向右后方突出压迫右侧L5神经根。诊断:腰椎间盘突出症(L4/5)。于2016年3月21日局麻下行椎间孔镜髓核摘除+纤维环汽化成形术,术后症状即刻缓解。复查CT示原突出髓核摘除彻底(图5)。术后3个月,门诊复查MRI示手术节段出现T2高信号,T1低信号类圆形影,11×6mm,未压迫神经根(图6),因患者无任何不适,予以观察,术后1年复查MRI,提示囊肿消失(图7)。

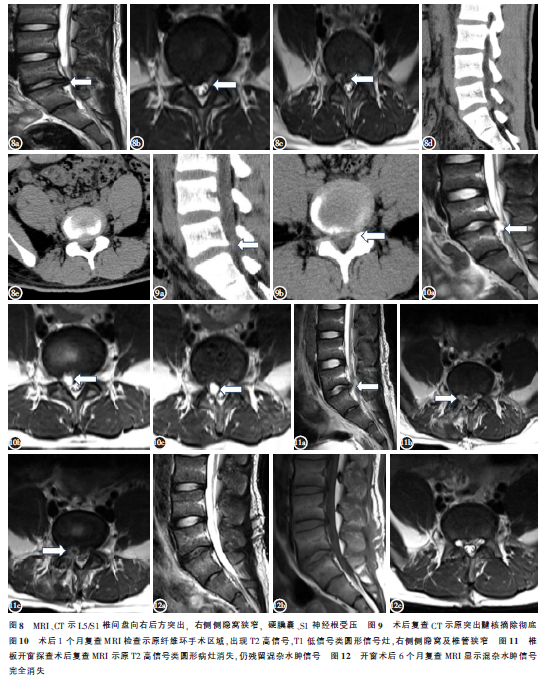
病例3,男性,16岁,“反复腰背部疼痛1年,伴右下肢疼痛7个月”入院。查体:右侧下肢S1根性痛。影像学:腰椎CT、MRI示L5/S1椎间盘向右后方突出,压迫S1神经根(图8)。诊断:腰椎间盘突出症(L5/S1)。于2017年10月11日连续硬膜外麻醉下行经椎板间入路脊柱内镜下髓核摘除+纤维环汽化成形术,术后患者症状即刻缓解。复查CT示突出髓核摘除彻底(图9)。术后1个月,再发腰背部及右下肢根性疼痛,基本同术前。复查MRI示原手术节段,出现T2高信号,T1低信号类圆形影,11×9mm,压迫右侧S1神经根(图10),予消炎止痛、脱水消肿等治疗2周后,症状无改善。经全科室讨论后,在全麻下行腰椎后路椎板开窗探查术。术中可见右侧S1神经根腹侧有一包裹性、暗黑色囊肿,术中完整切除,可见囊液为暗红色血性液体。术后疼痛症状改善。复查MRI示原高信号区消失,遗留混杂信号区,考虑为水肿信号(图11)。开窗术后6个月复查MRI,可见混杂水肿信号区消失(图12)。病理结果示囊壁为纤维结缔组织伴有新近和陈旧出血,未见椎间盘组织和上皮细胞,部分囊壁含有血管(图13)。

讨论
(一)临床病理特点。Young等于2009年首次报道了2例髓核摘除术后并发囊肿,因囊壁不完整,为与椎间盘囊肿区别,而命名为术后椎间盘假性囊肿(PDP)。PDP是一种罕见的PELD、MED、椎板切除髓核摘除术后并发症,Kang等报道的PELD术后PDP发生率为1%(1503例PELD患者术后发生15例PDP)。Ryutaro等报道的PDP发生率则仅为0.28%(359例PELD患者术后发生2例PDP)。Chiba等于2001年首次将囊内容物与椎间盘相通的椎管内髓外囊肿命名为椎间盘囊肿(discalcyst),并总结了其特点。其后Shiboi等撰文认为,PDP也具备椎间盘囊肿的特点:(1)与椎间盘突出症相似的根性症状;(2)好发于亚洲人群,尤其是年轻男性;(3)累及的椎间盘的退变较轻微;(4)椎间盘造影证实,囊肿与椎间盘有蒂相连通;(5)囊液多为血性液体或血清;(6)病理切片发现囊壁多为纤维结缔组织,可见炎性细胞浸润或炎性肉芽组织增生,有时可见含铁血黄素沉积,缺乏椎间盘组织和上皮细胞;(7)MRI在囊肿的诊断和鉴别诊断上有很高的价值———MRI显示椎间盘周围T1加权像低信号、T2加权像高信号的囊性结构,增强扫描可见囊壁环形强化。
笔者在Pubmed以“discalpseudocyst”、“annularpseudocyst”检索出6篇英文文献,其中欧美文献1篇,亚洲文献(日本、韩国、印度)5篇。在中国知网和万方平台以“椎间盘假性囊肿”检索出1篇中文文献。7篇文献及本组共报道39例PDP。其中,94.87%(37例)的患者为亚洲患者(主要是中、日、韩,共36例),均为PELD、MED术后并发PDP。仅有5.13%(2例)的患者为欧美患者,且均为椎板切除髓核摘除术后并发PDP,无1例PELD、MED术后的病例。说明PDP好发于亚洲人群。Chung等报道了12例PDP病例,文中依据术后MRI证实PDP存在的检查时间来计算PDP的形成时间,PELD术后并发PDP的平均时间约为1个月。我们根据相同方法统计了文献报道的39例病例,则PDP的平均形成时间约为61d,而剔除2例欧美椎板开窗术后PDP的病例后,PELD、MED术后并发PDP的平均时间则为42d,与Chung报道基本一致。然而,部分无症状患者是常规术后复查时才发现PDP的存在,其实PDP早已形成。有症状患者则会更早来院复查而相比无症状患者更早发现PDP。所以,文献报道的PDP形成时间仅供参考,并不能真实反映术后形成PDP的真实时间。笔者结合研究和相关文献报道,认为PDP形成于PELD、MED术后早期。
最易发生PDP的节段,临床尚无定论。复习文献39例病例,发生于L4/5节段有21例,占所有节段的53.84%;L5/S1节段有15例,占38.46%;L3/4节段占7.69%。若依据以上结果,说明L4/5节段的PDP发生率可能高于其他节段,但该结果仅在两个节段的手术病例数相等情况下才有意义。Kang等则回顾性分析了1503例PELD治疗的病例,其中L4/5节段1118例,采用椎间孔镜治疗,发生6例PDP,发病率0.54%;L5/S1节段330例,采用椎板间入路PELD治疗,发生9例PDP,发病率2.73%;其他节段55例,无PDP。结果说明椎板间入路(L5/S1)可能更易发生PDP(P<0.05)。Kang在文中提出,椎板间入路需要分离黄韧带、硬膜囊结构方能暴露病变椎间盘后缘,甚至可能损伤后纵韧带结构,对组织干扰和损伤较多,这可能是L5/S1发病率较高的可能原因。我们报道的3例病例,1例是椎间孔入路,2例是椎板间入路,我们亦倾向Kang的观点,认为L5/S1节段可能更容易术后并发PDP。然而,关于PDP的好发节段及相应的原因,需要进一步的回顾性分析甚至队列研究去证实。这是我们下一步努力的方向。
(二)PDP的发病机制。PDP的发病机制仍存在争议。考虑到PDP与椎间盘囊肿如此多的相似性,我们认为两者是同源性疾病,PDP是椎间盘囊肿的特殊类型,两者的发病机制有许多相同之处,所以Chung引用了椎间盘囊肿文献,分析PDP的可能发病机制,同时PDP可以帮助学者从创伤机制方面解释椎间盘囊肿的形成原因。Toyama和Chiba提出一种假说:椎间盘损伤或椎管内血管破裂形成囊肿。Toyama等报告7例囊肿中有4例囊液为血性液体,据此推测可能是椎间盘损伤后盘内出血引起囊肿,或是椎管内静脉丛撕裂引起硬膜外血肿,血肿吸收演变成囊肿;Chiba等回顾性分析8例椎间盘囊肿,认为囊肿的形成与椎间盘损伤相关。Chung和Young等提出另一种假说,认为突出的椎间盘诱发炎症反应,肉芽组织包绕在纤维环表面形成假膜,PELD摘除髓核过程中破坏了部分纤维环,但没有摘除纤维环外面的假膜,术后患者的轴性负荷挤压椎间盘内的液体、血液外渗,与假膜共同形成PDP(图14)。Kang等认为,PELD术中电凝止血、汽化成形等操作引起炎症反应,而椎板间入路则会损伤后纵韧带,加重了后纵韧带、纤维环及周围组织之间的炎症反应,从而诱发PDP。邱小明等在1例PDP的囊壁发现髓核样组织,提出新的假说:后部纤维环损伤后,髓核向后突出与周围纤维环一起形成膜状结构,封闭纤维环裂隙,而纤维环内部形成囊性空腔,血液和髓核内溢出液体在此空腔积聚形成假性囊肿。
临床实践发现,术后复查MRI时,部分患者会出现明显的T2相混杂信号影(图15),该信号影形态上与突出的髓核相似,但与髓核特征性的T2相低信号不同。此类患者术前症状均已缓解无复发,排除术后髓核再次突出,我们认为此类信号影为术区炎性水肿的表现。该现象可以佐证Young的假说,所以我们更倾向于Young的表述。
(三)治疗方法。PDP的治疗仍有争议。文献报道的39例PDP,保守治疗20例,手术治疗18例(CT引导穿刺抽液2例,PELD、MED、开窗髓核摘除16例),1例方案不明。20例保守治疗中3例无疗效评价,14例评价为优良,优良率为82.35%(优10例,良4例)。18例手术治疗中2例无疗效评价,15例评价优良,优良率为83.75%(优13例,良2例)。文献报道的保守和手术疗效让人满意。本组中病例2经保守治疗1年后复查,囊肿消失,说明部分PDP病例有自限性、自愈倾向,这可能是保守治疗有效的重要原因。邱小明解释了PDP的自限性:PDP由于囊壁结构不完整,且随着囊肿的增大而变薄,其自发吸收的可能性比较大。根据文献总结及我们的治疗经验:对于无症状性PDP的患者,定期复查MRI,囊肿可自然消退。对于症状性PDP的患者,应首先采取积极保守治疗,采取口服消炎镇痛、脱水消肿、甲钴胺营养周围神经等治疗。对于经积极保守治疗后症状无缓解或加重者,可以考虑予以外科治疗。手术方案可以考虑在CT引导下穿刺抽吸+抗炎药物封闭治疗(Young等);也可以采用PELD、MED予以囊肿清除(邱小明等);也可以像我们的病例3采用椎板开窗囊肿切除的治疗方法。外科手术疗效确切,治愈率和优良率高。
结论PDP为脊柱内镜术后罕见并发症,多为术后40d左右出现,症状体征与腰椎间盘突出复发相似,而临床病理和影像学则与椎间盘囊肿相似。PDP和椎间盘囊肿可能是同源性疾病。鉴别PDP和椎间盘突出复发主要依靠MRI。建议PDP首选保守治疗,效果不佳再行外科治疗。外科治疗效果确切。目前仍需要进一步的研究揭示其形成机制。
原始出处:
吴环宇,张明彦,刘向阳,沈雄杰,常磊,刘斌,彭帅.经皮内窥镜下腰椎间盘切除术后并发假性囊肿3例报道[J].中国脊柱脊髓杂志,2019,29(05):475-480.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#假性囊肿#
37
#切除术#
31
#并发#
27
#腰椎#
31
#囊肿#
40
#内窥镜#
37
#腰椎间盘#
35