Neurology:老年颈动脉夹层患者更易误诊
2017-03-20 MedSci MedSci原创
目的:在一组诊断为颈动脉夹层的患者(CeAD),确定年龄≥60岁患者的比例,并且比较年龄≥60岁及<60岁患者的特征的频率特性(症状、危险因素和预后)。方法:研究者结合确诊为CeAD的三大队列研究中患者的数据(即颈动脉夹层与缺血性卒中患者联盟)。研究者将病例分为年龄≥60岁和<60岁这两组,并比较两组间临床特点、危险因素、血管特征及3个月预后。首先,研究者对汇集个别病人的数据进行汇总分析。在每个队
目的:在一组诊断为颈动脉夹层的患者(CeAD),确定年龄≥60岁患者的比例,并且比较年龄≥60岁及<60岁患者的特征的频率特性(症状、危险因素和预后)。
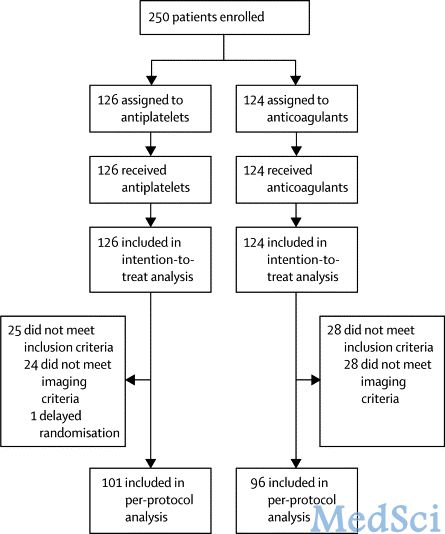
方法:研究者结合确诊为CeAD的三大队列研究中患者的数据(即颈动脉夹层与缺血性卒中患者联盟)。研究者将病例分为年龄≥60岁和<60岁这两组,并比较两组间临床特点、危险因素、血管特征及3个月预后。首先,研究者对汇集个别病人的数据进行汇总分析。在每个队列和跨队列进行二次分析。计算粗和校正比值比OR (95%CI)。
结果:确诊的CeAD的患者共2391例,年龄超过≥60岁的患者177例(7.4%)。在这个年龄组,颈部疼痛(校正OR 0.47 [ 0.33-0.66 ])、头痛(校正 OR 0.58 [ 0.42-0.79 ]),机械性触发事件(校正OR 0.53 [ 0.36-0.77 ])和偏头痛(校正OR 0.58 [ 0.39-0.85 ])的发生率比年轻患者频繁。反过来,老年患者高胆固醇血症(校正OR1.52 [ 1.1-2.10 ])和高血压(校正OR 3.08 [ 2.25-4.22 ])更为常见。二级分析中证实年龄组间的主要差异。在多变量分析中,校正分析,老年组患者良好预后(校正OR 0.45 [ 0.25,0.83 ])(即,改良Rankin量表评分0-2)较少见。
结论:在确诊为CeAD的患者中,年龄≥60岁的比例为1/14。在这些患者中,疼痛和机械触发可能较少,使诊断更具挑战性,增加了老年患者漏诊CeAD的风险。
原文出处:
Traenka C, Dougoud D, et al. Cervical artery dissection in patients ≥60 years: Often painless, few mechanical triggers. Neurology. 2017 Mar 3.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Neurol#
31
#颈动脉夹层#
36
#颈动脉#
25
#动脉夹层#
28