Int Arch Otorhinolaryngol:耳蜗植入前评估:重度双侧舌前听力损失儿童的临床资料和家族史
2020-11-07 AlexYang MedSci原创
巴基斯坦的耳聋患病率高。对深度听力损失患者的临床特征的了解不仅有助于查明原因,也有助于公共卫生干预措施的策略规划。
巴基斯坦的耳聋患病率高。对深度听力损失患者的临床特征的了解不仅有助于查明原因,也有助于公共卫生干预措施的策略规划。
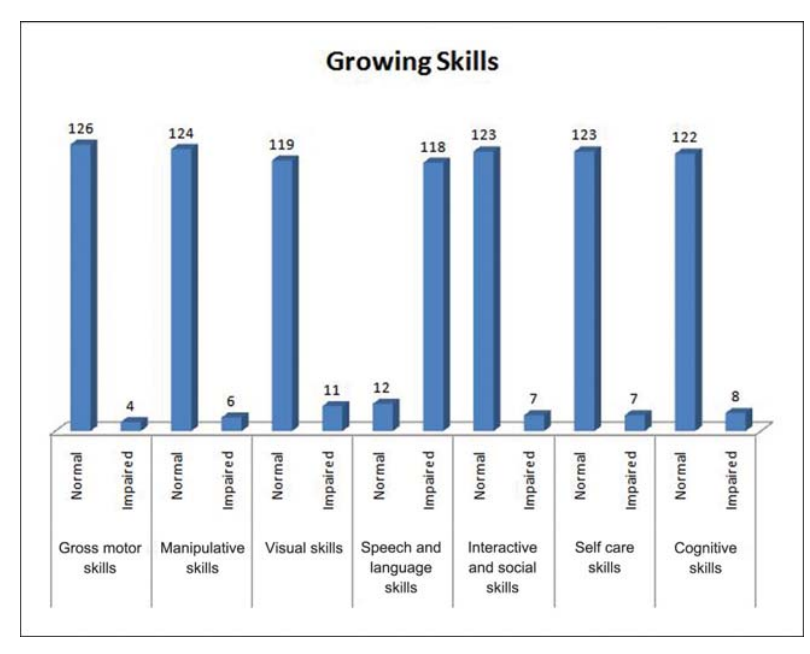
最近,有研究人员调查了听力损失儿童的临床情况,即发病年龄、相关缺陷和障碍、可能的病因、相关家族史以及近亲结婚的影响。研究自2016年11月至2018年9月进行。研究人员将所有6岁以下的双侧深度听力损失、且将会受益于人工耳蜗植入术的儿童患者纳入了研究。研究详细记录了病史,并对患者各方面的发育能力进行了评估。根据Schedule of Growing Skills II对患者的运动能力、操作能力、视觉能力、语言能力、社交能力和自理能力进行评分。研究人员还对患儿父母进行了详细的家族史调查。研究表明,待治疗患儿的平均年龄为3.2±1.25岁。大多数患者(51.5%)有阳性家族病史。近亲结婚很常见;76.9%的患者的父母是一级亲属。大多数患者(90.8%)有相关语言障碍。总共有4名(Ł3.07%)患者有全局性发育迟缓。
最后,研究人员指出,近亲结婚在该疾病的发展过程中具有重要作用。这些儿童的发育与会诊的年龄紧密相关。
原始出处:
Syed Hashim Raza , Rehmana Waris , Samina Akhtar et al. Precochlear Implant Assessment: Clinical Profile and Family History of Children with Severe Bilateral Prelingual Hearing Loss. Int Arch Otorhinolaryngol. Oct 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习!
80
#听力#
37
#家族史#
38
#植入#
35
#双侧#
34
#耳蜗植入#
33
学习
86