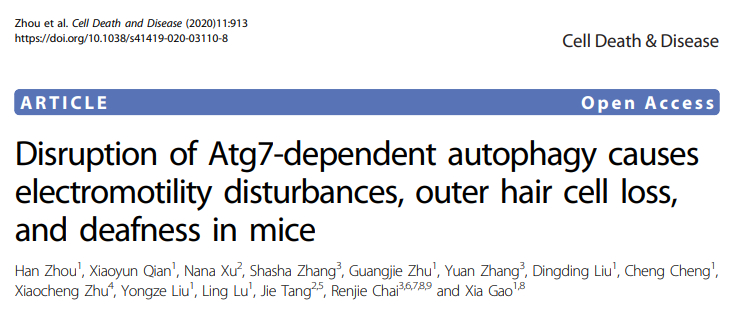
Cell Death Dis:Atg7依赖性自噬的破坏导致电能动性干扰、外毛细胞丢失和耳聋
2020-11-07 AlexYang MedSci原创
Atg7是一个不可缺少的因子,在典型的非选择性自噬中起着重要作用。
Atg7是一个不可缺少的因子,在典型的非选择性自噬中起着重要作用。
最近,有研究人员表明,小鼠外毛细胞(OHCs)中Atg7的基因敲除会随着时间的推移引起立体声损伤、体细胞电能动性干扰和突触前带状物的退化,进而导致OHCs逐渐大规模丧失和随后的早发性深度听力损失。自噬功能受损破坏了OHC线粒体功能,引起功能障碍线粒体的积累;正常情况下,功能障碍线粒体能够被及时的清除。与Atg7无关的自噬/线粒体过程不能弥补Atg7的缺失,也不能挽救终末分化的非增殖性OHCs。
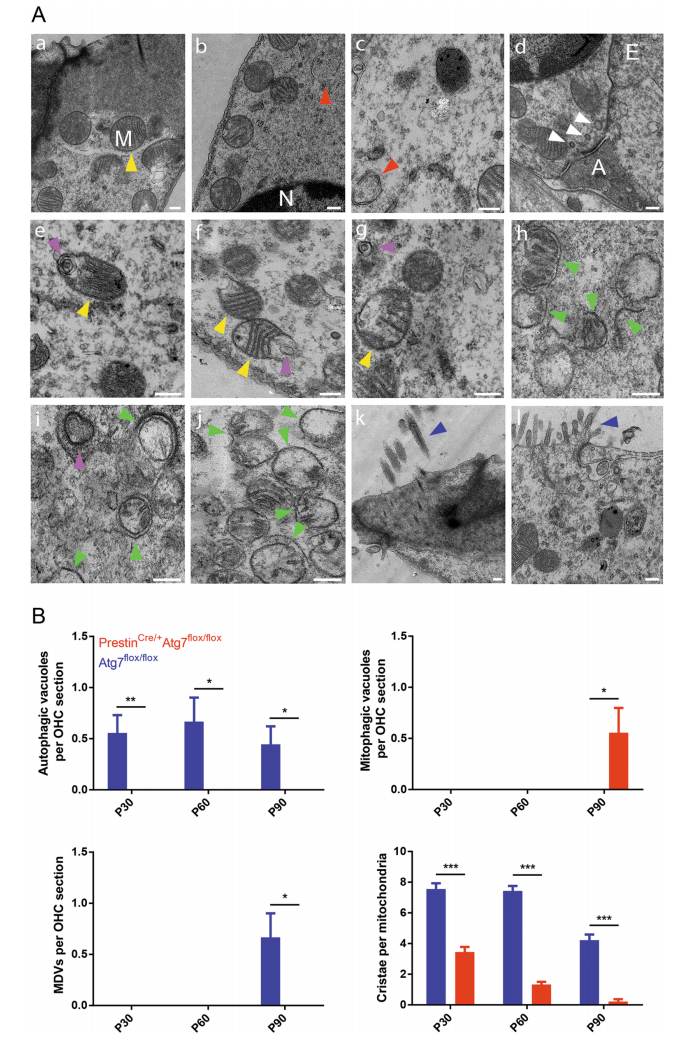
Atg7缺陷OHCs和对照OHCs的TEM显微照片
最后,研究人员指出,OHCs协调了复杂的非选择性和选择性自噬/裂解途径,并协同工作来维持细胞稳态。总的来说,他们的结果表明了Atg7依赖性自噬在保护OHCs和维持听力功能方面起着关键的细胞保护作用。
原始出处:
Han Zhou, Xiaoyun Qian, Nana Xu et al. Disruption of Atg7-dependent autophagy causes electromotility disturbances, outer hair cell loss, and deafness in mice. Cell Death Dis. Oct 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#外毛细胞#
44
#Cell#
34
#Dis#
50
#CEL#
43
学习
70
#Death#
0