Science Signaling:体外化疗“打残”癌细胞,结合免疫疗法消灭肿瘤,无复发
2021-10-21 医诺维 医诺维
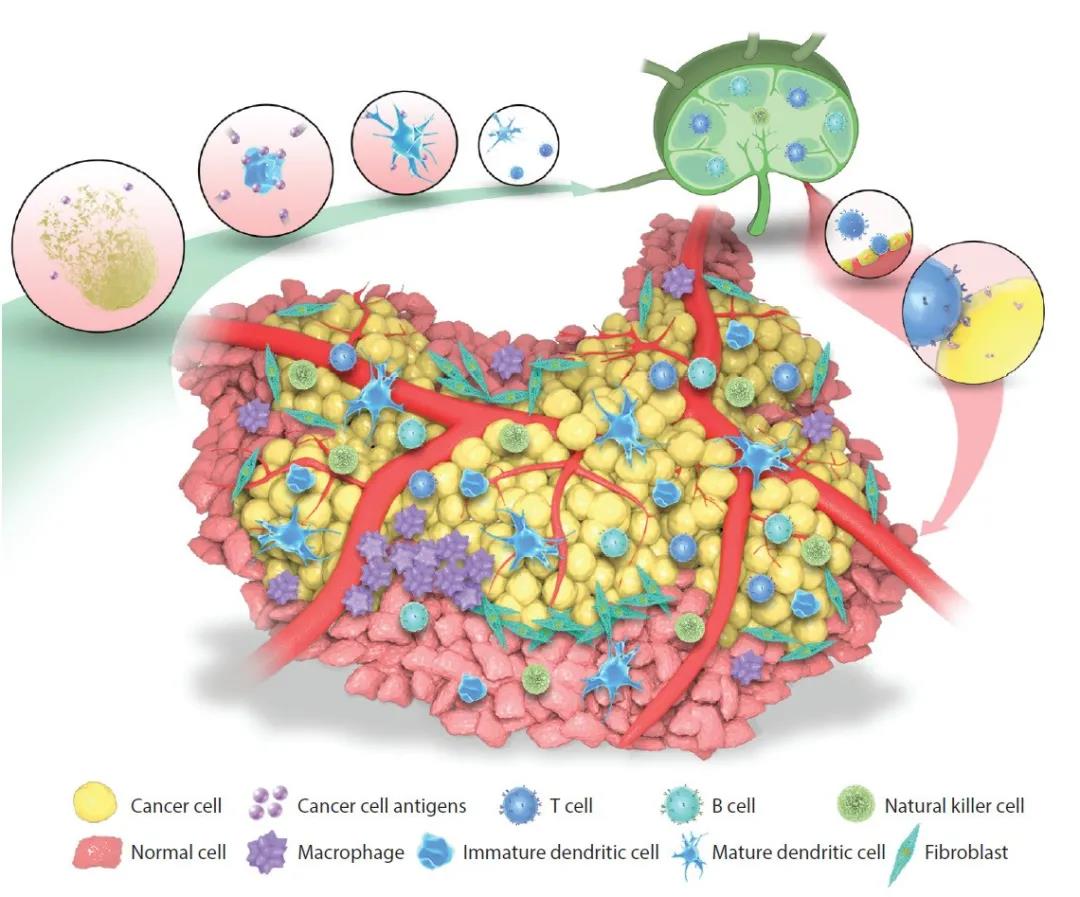
近年来,肿瘤免疫治疗的发展迅速,为人类彻底攻克癌症带来了新的希望,但它只对少数癌症有效。免疫疗法是通过人体自身的免疫系统来攻击癌症,但大多数肿瘤会产生高度免疫抑制的环境,使T细胞失活。然而,免疫检查点
近年来,肿瘤免疫治疗的发展迅速,为人类彻底攻克癌症带来了新的希望,但它只对少数癌症有效。免疫疗法是通过人体自身的免疫系统来攻击癌症,但大多数肿瘤会产生高度免疫抑制的环境,使T细胞失活。然而,免疫检查点疗法的工作原理是使T细胞恢复活力,从而摧毁肿瘤。
2021年10月19日,美国麻省理工学院的研究人员在" Science Signaling "期刊发表了一篇题为" The injury response to DNA damage in live tumor cells promotes antitumor immunity "的研究论文。
研究人员发现了一种治疗肿瘤的新方法,利用受损的肿瘤细胞唤醒免疫系统攻击肿瘤,在小鼠模型中,该疗法可以完全消除近一半小鼠的肿瘤。
目前用于癌症免疫治疗的一类药物是检查点阻断抑制剂,它可以阻止已经耗尽且无法攻击肿瘤的 T 细胞。这些药物在治疗几种类型的癌症方面取得了成功,但对许多其他类型的癌症无效。
在该研究中,研究人员尝试通过将这些药物与细胞毒性化疗药物结合来提高它们的性能,希望化疗可以帮助刺激免疫系统杀死肿瘤细胞。
研究人员首先用几种不同的化疗药物以不同的剂量治疗离体的癌细胞。24小时后,研究人员在每个培养皿中加入树突细胞,24小时后加入 T 细胞。然后,测量了 T 细胞杀死癌细胞的能力。
令人惊讶的是,研究人员发现大多数化疗药物并没有起到多大作用,而那些有助于治疗的药物似乎在低剂量、不会杀死很多细胞的情况下效果最好。
所以,研究人员表示,并不是死的肿瘤细胞刺激了免疫系统,相反,关键因素是因化疗而受伤但仍然存活的癌细胞。
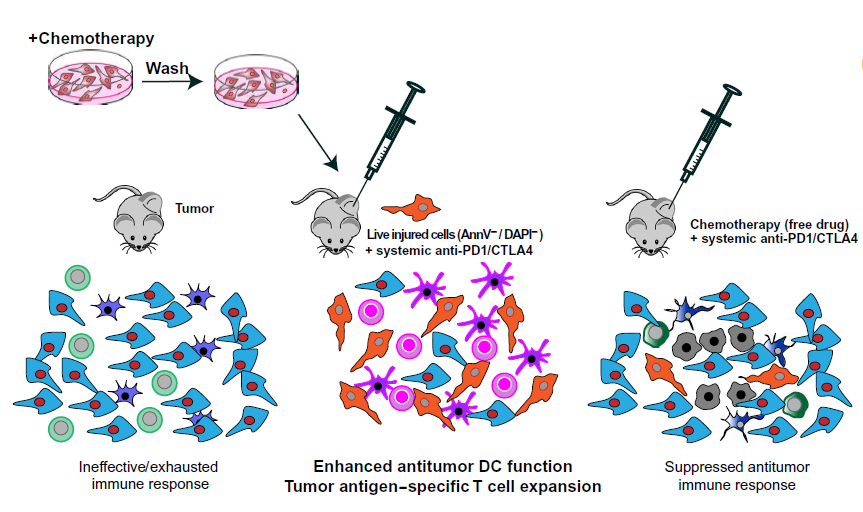
体外培养,注入体内,与全身免疫检查点阻断结合激活免疫系统
此外,研究人员发现,最有效的药物是能引起DNA损伤的药物,因为当肿瘤细胞发生DNA损伤时,它激活了对压力作出反应的细胞通路。这些通路发出求救信号,刺激T细胞迅速行动,不仅摧毁受伤的细胞,而且摧毁附近的任何肿瘤细胞。

DNA损伤的肿瘤细胞介导 T 细胞反应
在患有黑色素瘤和乳腺肿瘤的小鼠模型中,这种疗法在40%的小鼠体内完全消除了肿瘤。
不仅如此,当研究人员在几个月后将癌细胞注射到这些小鼠体内时,小鼠的T细胞在它们形成新的肿瘤之前识别并消灭它们,不再复发。
研究人员还尝试将破坏DNA的药物直接注射到体内肿瘤中,而不是体外的细胞,但他们发现这并不有效,因为化疗药物还会伤害肿瘤附近的 T 细胞和其他免疫细胞。此外,在没有检查点阻断抑制剂的情况下注射受损细胞也没有效果。
总之,该研究描述了一种新的癌症治疗方法,利用化疗药物加免疫治疗,最终完全消除肿瘤,并且具有长期抗肿瘤免疫记忆,不再复发。
最后,研究人员希望在肿瘤对免疫疗法没有反应的患者中测试这种方法,但首先需要更多的研究来确定哪些药物和剂量对不同类型的肿瘤最有益。研究人员还在进一步研究受伤的肿瘤细胞究竟是如何刺激如此强烈的 T 细胞反应的细节。
原始出处:
GANAPATHY SRIRAM LAUREN E. MILLING JUNG-KUEI CHEN, et al. The injury response to DNA damage in live tumor cells promotes antitumor immunity. SCIENCE SIGNALINGVOL. 14, NO. 70519 OCT 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Signal#
38
#signaling#
44
#Sign#
47
很有意思,这个值得探寻,也说明我们在临床治疗中,可能并不需要太多的太强的化疗药物。
88
#癌细胞#
32
#SCIE#
24
学习
72