J Hepatology:熊去氧胆酸(UDCA)治疗原发性胆源性胆管炎的疗效分析
2020-09-12 MedSci原创 MedSci原创
肝移植(LT)后原发性胆源性胆管炎(PBC)的复发很常见,它可能会损害肝脏移植物和患者的生存时间。熊去氧胆酸(UDCA)是目前PBC的标准疗法。
背景与目标
肝移植(LT)后原发性胆源性胆管炎(PBC)的复发很常见,它可能会损害肝脏移植物和患者的生存时间。熊去氧胆酸(UDCA)是目前PBC的标准疗法。本项研究旨在调查预防性使用UDCA对LT后PBC复发的发生率和长期后果的影响。
方法
1983-2017年间,研究人员在16个研究中心(9个国家)对780例因PBC行肝移植的患者进行了回顾性队列研究,平均随访11年。其中,有190人接受了预防性UDCA(10-15 mg / kg /天)治疗。主要结局是PBC复发的组织学表现,肝相关死亡和全因死亡。预防性UDCA与预后之间的关联使用多变量调整的Cox模型和受限平均生存时间(RMST)模型进行了量化。
结果
尽管PBC的复发显着缩短了肝移植物和患者的生存期,但预防性使用UDCA与PBC复发的风险降低([aHR] 0.41; 95%CI 0.28-0.61;p < 0.0001),移植物丢失(aHR 0.33; 95%CI 0.13-0.82; p < 0.0001),肝脏相关死亡(aHR 0.46; 95%CI 0.22-0.98; p < 0.05)和全因死亡(aHR 0.69; 95%CI 0.49-0.96; p < 0.05)有关。在RMST分析中,预防性使用UDCA可以在20年内获得2.26年的生存期(95%CI 1.28–3.25)。暴露于环孢素而不是他克莫司具有预防性UDCA的补充保护作用,从而减少了PBC复发和全因死亡的累积发生率。
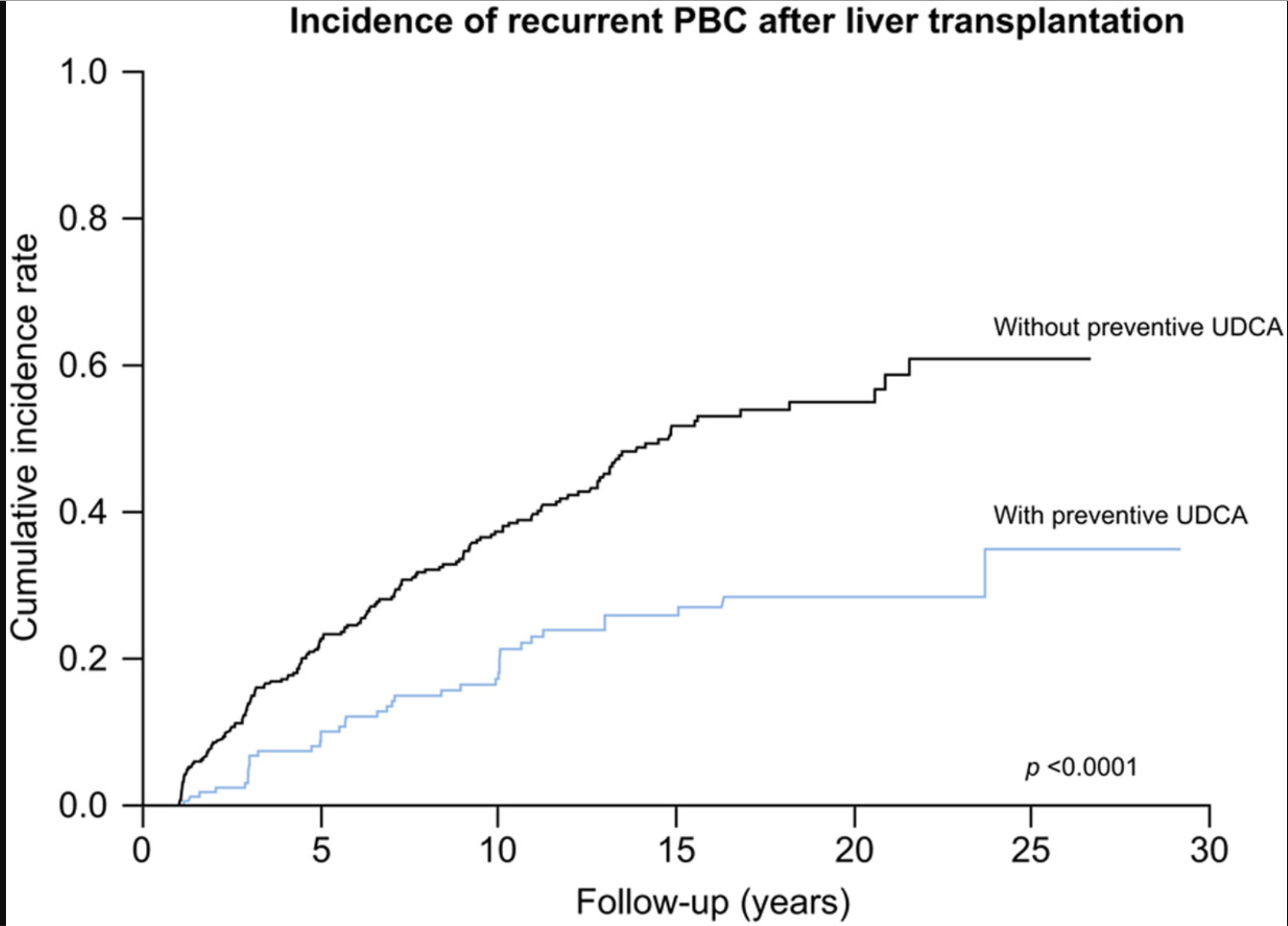
结论
因PBC行肝移植后的预防性使用UDCA与疾病复发,肝移植物损害和死亡的风险降低有关。联合使用环孢素和预防性UDCA的方案可使PBC复发和死亡的风险最低。
原始出处:
Christophe Corpechot. Et al. Long-term impact of preventive UDCA therapy after transplantation for primary biliary cholangitis.Journal of Hepatology.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#疗效分析#
28
#原发性#
35
#UDCA#
34
#熊去氧胆酸#
35
#EPA#
38
#胆管#
22
好
78
谢谢梅斯提供这么好的信息,学到很多
51
T_T
82