



本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
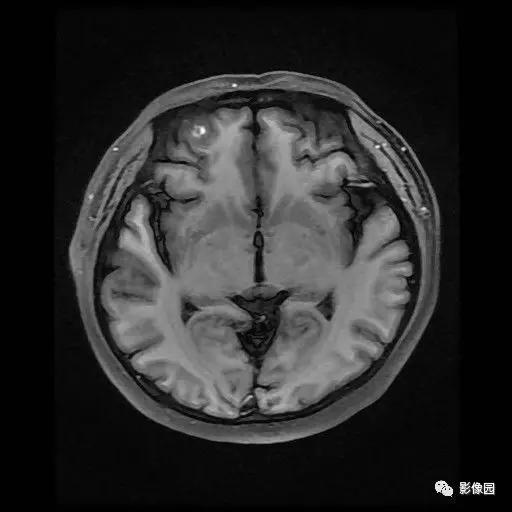
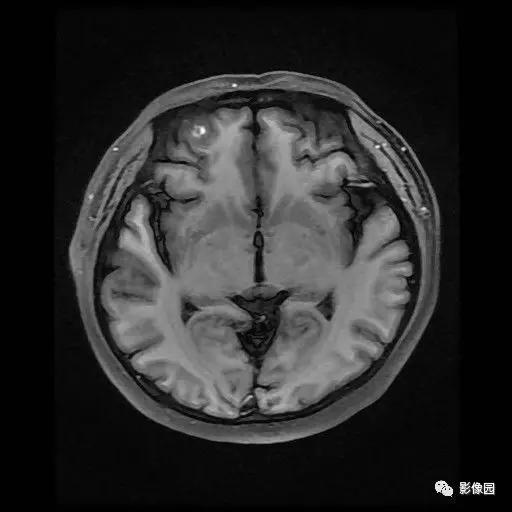


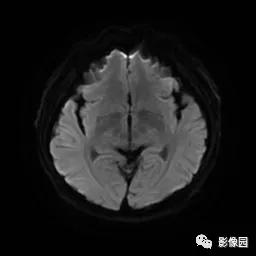


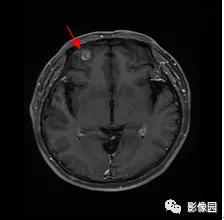

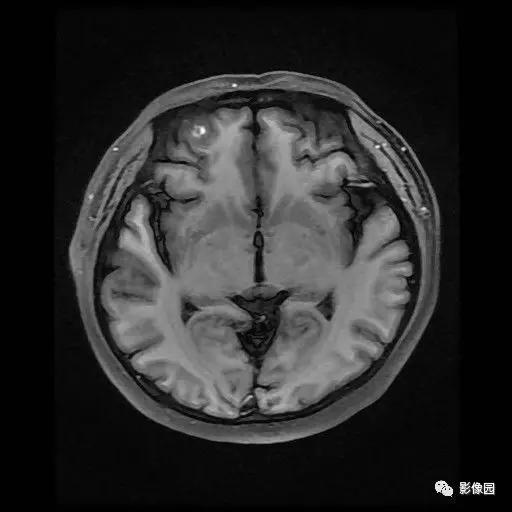
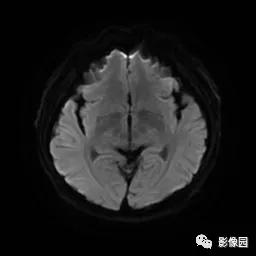
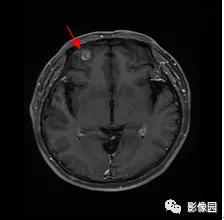
脑海绵状血管畸形(Cerebral cavernous malformations,CCM),也称为海绵状血管瘤,是一种常见的颅内血管异常。其中1/5的患者超过1个 CCM,普通人群的发病率大约为0.1%-0.5%。排在颅内动脉瘤以后,CCM 是第二常见的脑血管畸形。
患者男,48岁,因“渐进性双下肢麻木、无力1年,加重6个月”于2017年10月14日收住院。10年前因高处坠落伤致T4椎体压缩性骨折(图1a,b),伤后即感胸背部持续性钝痛,躯干及四肢感觉运动正常,经卧床休息等非手术治疗3个月后恢复正常生活。近1年出现感觉减退,由双下肢远心端向近心端渐进性发展,近10d发现双下肢渐进性无力,可站立、行走。查体示双侧肋弓以下平面痛、温觉及触觉减退,双下肢肌力4级,肛
患儿,男,5个月。患儿母亲(29岁)在怀孕37周时,行腹部B超检查发现胎儿右侧额叶脑实质内有一4.4 cm×3.4 cm大小的偏强回声,呈现点条状血流信号,其周围可见大小4.6 cm×3.2 cm的液性暗区(图1);胎心140次/min,生命体征平稳。在山东省千佛山医院行腹部MRI检查示:胎儿一侧侧脑室旁可见一不规则形短T1长T2异常信号,信号不均匀(图2);诊断为额叶占位并囊性病变。考虑良性病变
患者男,57岁,因“右侧阵发性耳鸣”来院就诊;颅脑CT平扫示右侧桥小脑角区见不规则软组织密度影,CT值约37Hu,大小约2.8 cm×1.2 cm,密度不均匀,其内见斑结状稍高密度影(CT值约50Hu),邻近脑组织稍受压,右侧内听道较左侧略增宽(图1)
患者男,28岁。因黑便半年,头晕、乏力2个月余来我院就诊。曾在外院予以输血及补充铁剂等治疗,头晕乏力症状改善。实验室检查:白细胞计数4.29×109/L,血红蛋白88.0g/L,血小板计数307×109/L。
云南省第二人民医院眼科的Li J近日在Curr Eye Res杂志上发表了一篇重要的工作,他们研究了视网膜海绵状血管瘤(RCHs)的多模态成像特征。


梅斯医学MedSci APP
医路相伴,成就大医
学习
56
很好
67
#头晕#
30
#恶心#
25