J Thorac Oncol:放疗分割方式是否与脑转移相关?III期临床研究CONVERT给你答案
2019-02-19 肿瘤资讯 肿瘤资讯
2018年6月《柳叶刀·肿瘤》(The Lancet Oncology)公布了Ⅲ期临床研究CONVERT的研究结果,该研究继续支持超分割放疗联合化疗是局限期小细胞肺癌胸部放疗的标准模式。目前,还没有前瞻性研究评估局限期小细胞肺癌患者接受预防性颅脑照射(PCI)后剂量和分割方式对脑转移风险的影响。英国Corinne Faivre-Finn 教授团队进行了前瞻性Ⅲ期CONVERT 研究的二次分析,研究
1999年,发表于《新英格兰医学杂志》(New England Journal of Medicine)的前瞻性临床研究INT 0096奠定了超分割放疗联合化疗作为局限期小细胞肺癌(LS-SCLC)标准治疗的地位。2018年6月《柳叶刀·肿瘤》(The Lancet Oncology)公布了Ⅲ期临床研究CONVERT的研究结果,该研究继续支持超分割放疗联合化疗是局限期小细胞肺癌胸部放疗的标准模式。目前,还没有前瞻性研究评估局限期小细胞肺癌患者接受预防性颅脑照射(PCI)后剂量和分割方式对脑转移风险的影响。英国Corinne Faivre-Finn 教授团队进行了前瞻性Ⅲ期CONVERT 研究的二次分析,研究结果近期刊登在《胸部肿瘤学杂志》(Journal of Thoracic Oncology)上。
研究背景
小细胞肺癌的特点之一是癌细胞倍增时间短,因而在其自然病史中易发生脑转移。已有研究显示,预防性颅脑照射可以降低局限期小细胞肺癌患者发生脑转移的风险。在两项荟萃分析中,对放化疗应答且一般状态评分(PS)较好的患者,接受预防性颅脑照射会产生总生存的绝对获益。因此,预防性颅脑照射也被认为是这部分患者标准治疗的一部分。
但关于脑预防性照射仍有很多悬而未决的问题。第一,目前两项荟萃分析涉及的研究是在脑磁共振成像(MRI)成为小细胞肺癌的标准监测之前进行的,而脑MRI在预防性颅脑照射在中的作用尚不确定。第二,即使支持尽早进行预防性颅脑照射,也无法确定放化疗后进行预防性颅脑照射的最佳时机。第三,还没有前瞻性评估分析胸部放射治疗(RT)的剂量和分割方式对脑转移发生风险的影响。理论上,加速超分割放射治疗可以通过缩短治疗时间来降低治疗过程中肿瘤细胞再生的风险。
研究方法
CONVERT是一项多中心Ⅲ期临床研究,纳入根据美国东部肿瘤协作组体力状况量表(ECOG-PS)评分为0~2的局限期小细胞肺癌患者,随机分配接受放射治疗。从化疗(4~6个周期的顺铂+依托泊苷)第2周期开始,每天接受2次(45Gy,1.5Gy/f)或1次(66Gy,2Gy/f)放疗。随机分组前4周内必须进行脑部CT或MRI检查,化疗后无疾病进展和无脑转移(BM)患者接受预防性颅脑照射治疗。
该研究分析评估了Ⅲ期CONVERT研究中接受预防性颅脑照射治疗的患者数据。从开始接受预防性颅脑照射治疗到首次复发或死亡,分别评估脑复发时间和总生存(OS)的预测因子。采用Fine和Gray竞争风险模型评估脑复发率的预测因子,采用Cox比例风险模型分析评估OS的预测因子。
研究结果
2008年4月至2013年11月期间,研究收集来自8个国家73个中心的547例患者数据。分别有274例和273例患者接受每天2次BD放化疗(BD组)和每天1次OD 放化疗(OD组)。543例患者(BD组273例,OD组270例)进行了意向治疗分析,4例患者失访。其中,449例(83%)患者完成放化疗后接受了预防性颅脑照射治疗,BD组和OD组分别有81%(220/273)和85%(229/270)患者接受了预防性颅脑照射。根据美国癌症联合委员会/国际抗癌联盟(AJCC/UICC)分期标准,分别有Ⅰ期4例(1%),Ⅱ期74例(16%)和Ⅲ期346例(77%)患者接受预防性颅脑照射治疗患者,25例患者分期未知。
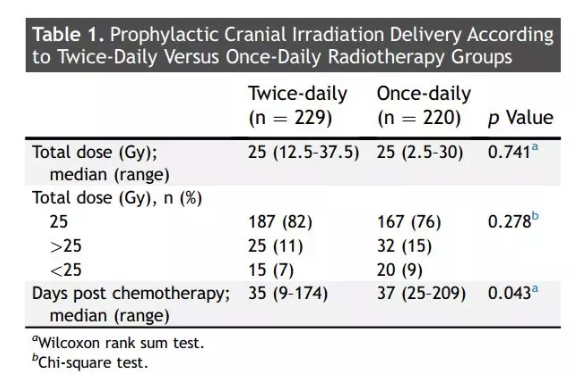
两组患者的中位预防性颅脑照射总剂量为25Gy(表1)。最后一个化疗周期后,与BD组(化疗后中位35天)相比,OD组化疗后中位37天给予预防性颅脑照射治疗(P<0.04)。但若从化疗开始时分析,两组患者接受预防性颅脑照射的时间无差异。
表1.OD组和BD组接受预防性颅脑照射治疗
中位随访45个月时,在接受预防性颅脑照射的患者中,75例(17%)患者出现了脑转移,其中OD组和BD组分别为16%(35/220)和17%(40/229),173例(39%)患者出现其他颅外进展。
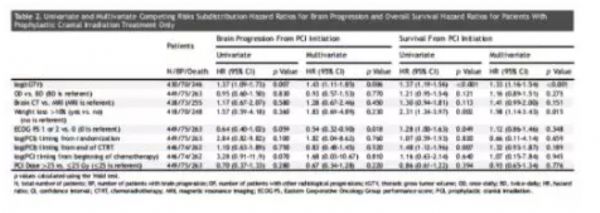
在单变量分析中,仅有胸部总肿瘤总体积(tGTV)与脑转移发生(HR=1.37,95%CI 1.09~1.73,P=0.007)及其他颅外进展(HR=1.43 95%CI 1.11~1.85, P=0.006)相关。而分割方式、预防性颅脑照射给予时间、预防性颅脑照射剂量、基线使用的成像方法(CT或MRI)与脑转移无关。在多变量分析中,tGTV和PS≥1与脑转移发生和其他颅外进展相关(表2)。
表2.单变量和多变量分析中脑转移和总生存的相关因素
预防性颅脑照射组的OS为29个月。BD组和OD组的中位OS分别为28个月和31个月。接受预防性颅脑照射的患者中,总人群、OD组和BD组的3年总生存率分别为45%、42%和48%。
在单变量分析中,化疗结束后接受预防性颅脑照射治疗的时间、体重减轻超过10%和tGTV是OS预后的预测因子。在多变量分析中,仅tGTV与OS相关。排除放化疗后疾病进展的患者,未接受和接受预防性颅脑照射治疗患者的中位OS分别为11.8个月和13.9个月(P<0.001)。
讨论和结论
由于可能存在神经心、理毒性的潜在风险,预防性颅脑照射治疗在局限期小细胞肺癌中的作用一直存在争议。
最近一项日本研究中,在积极进行脑部MRI影像学随访的广泛期小细胞肺癌患者中比较了接受预防性颅脑照射和观察患者的生存情况,该研究结果对欧洲癌症研究和治疗组织(EORTC)的治疗标准提出了质疑。在这项日本临床研究中,与观察组相比,预防性颅脑照射没有显示出更好OS,考虑也可能是某些因素影响了患者从预防性颅脑照射中获益。
最近来自美国的一项实践调查显示,98%的放射肿瘤学家在治疗前推荐预防性颅脑照射和96%推荐在行预防性颅脑照射之前行脑部MRI。但仍然需要更多的研究来指导和支持临床医师的决策。
CONVERT试验显示,肿瘤总体积较大与发生脑转移风险、其他颅外进展风险较高相关,而分割方式与脑转移风险无关。进一步完善预测模型将有助于实现更个性化的治疗。
参考文献
LEVY A, Le PÉCHOUX C, MISTRY H, et al. Prophylactic cranial irradiation for limited-stage small-cell lung cancer patients: secondary findings from the prospective randomized phase 3 CONVERT trial[J/OL]. J Thorac Oncol,2019,14(2):294-297.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






收藏
47
#II期临床研究#
27
#Oncol#
37
#THORAC#
39
#I期临床#
29
#III#
23
#III期临床研究#
36
#II期临床#
21
#III期#
32
看看
73