Stroke:急性缺血性卒中儿童血管内血栓切除术的疗效
2022-03-12 MedSci原创 MedSci原创
对接受EVT治疗的缺血性卒中儿科患者的临床病程和短期结局的横断面评估表明,EVT可能是一种安全的方式,可获得较高的良好功能结局。
关于儿童缺血性卒中后血管内血栓切除术(EVT)的使用和结局的证据有限,其使用的理由主要基于在成人中观察到的临床益处来推断。

近日,心血管疾病领域权威杂志Stroke上发表了一篇研究文章,研究人员查询了来自全国住院患者样本的加权出院数据,以确定2010年至2019年期间患有缺血性卒中(<18岁)的儿科患者。并使用复杂样本统计方法来归纳EVT治疗患者的概况和临床结局。研究人员根据EVT治疗患者和医疗管理患者之间基线特征的差异,进行倾向调整以解决EVT适应症引起的混杂情况。
在确定的7365名缺血性卒中儿童患者中,190名(2.6%)患者接受了EVT治疗。在EVT后临床试验时代,EVT治疗使用率显著增加(2016-2019;1.7% vs. 4.0%;P<0.001),而去骨瓣减压术的使用减少(2.8% vs. 0.7%;P<0.001)。在未经调整的分析中,105名(55.3%)患者接受EVT治疗的患者在出院时(回家或急性康复)取得了良好的功能结局,而没有报告围手术期医源性并发症或造影剂肾损伤的情况。倾向调整后,与药物治疗的患者相比,EVT治疗的患者表现出更高的绝对但不显著的有利功能结局发生率(55.3% vs. 52.8%;P=0.830;对于不利的结局调整后的风险比为1.01[95%CI为0.51-2.03];P=0.972)。
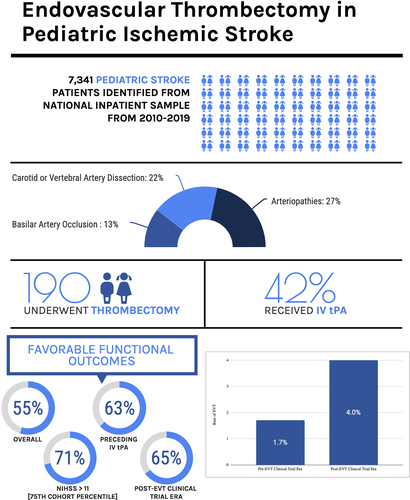
在美国国立卫生研究院卒中量表基线评分>11(队列评分的第75个百分位)的患者中,与仅接受药物治疗的患者相比,EVT治疗的患者倾向获得更高的有利功能结局(71.4% vs. 55.6%;P=0.146)。在对接受EVT治疗的患者进行的亚组评估中,在溶栓治疗之前接受过治疗的患者(n=79,41.6%)倾向于获得更高的有利功能结局发生率(63.3% vs. 49.5%;P=0.060)。
由此可见,对接受EVT治疗的缺血性卒中儿科患者的临床病程和短期结局的横断面评估表明,EVT可能是一种安全的方式,可获得较高的良好功能结局。
原始出处:
Alis J. Dicpinigaitis.et al.Endovascular Thrombectomy for Pediatric Acute Ischemic Stroke.stroke.2022.https://www.ahajournals.org/doi/10.1161/STROKEAHA.121.036361
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#缺血性卒#
32
#切除术#
30
#缺血性#
41
#血栓切除#
40
#血栓切除术#
51
#血管内血栓切除术#
38