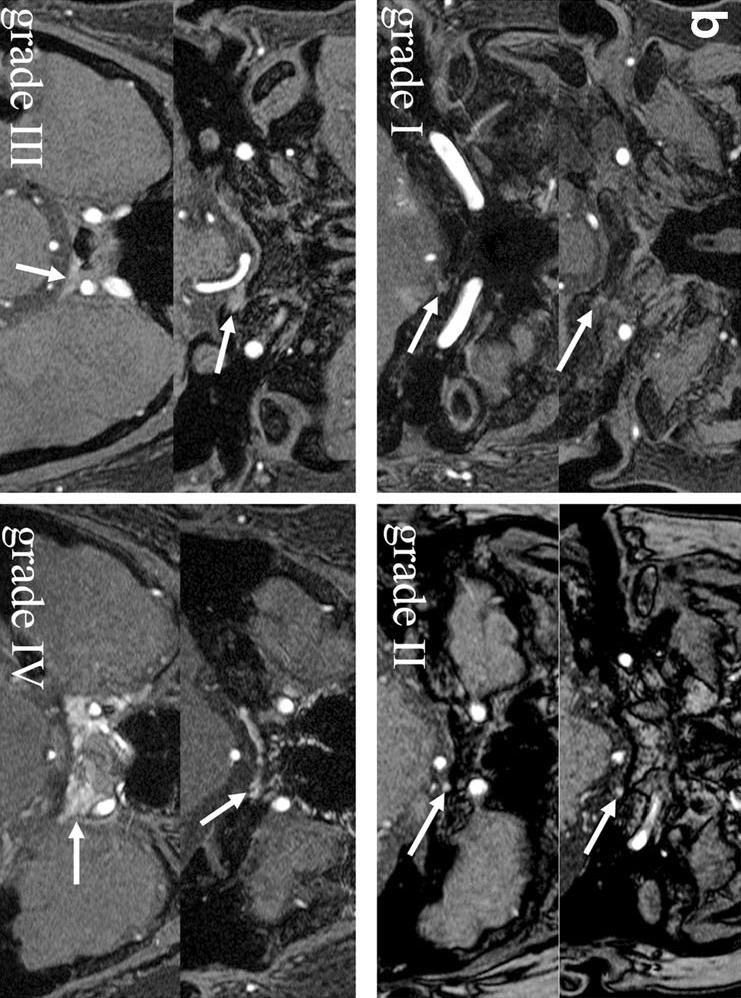
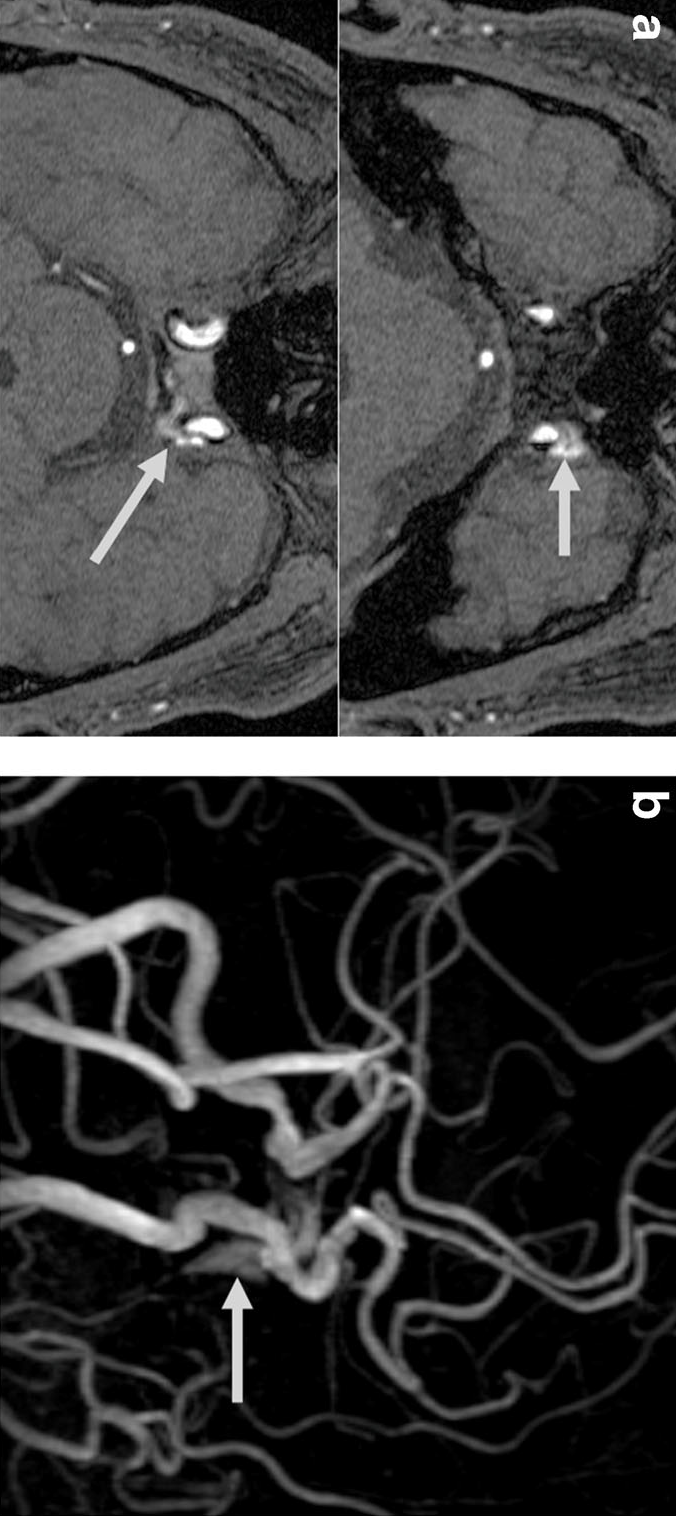
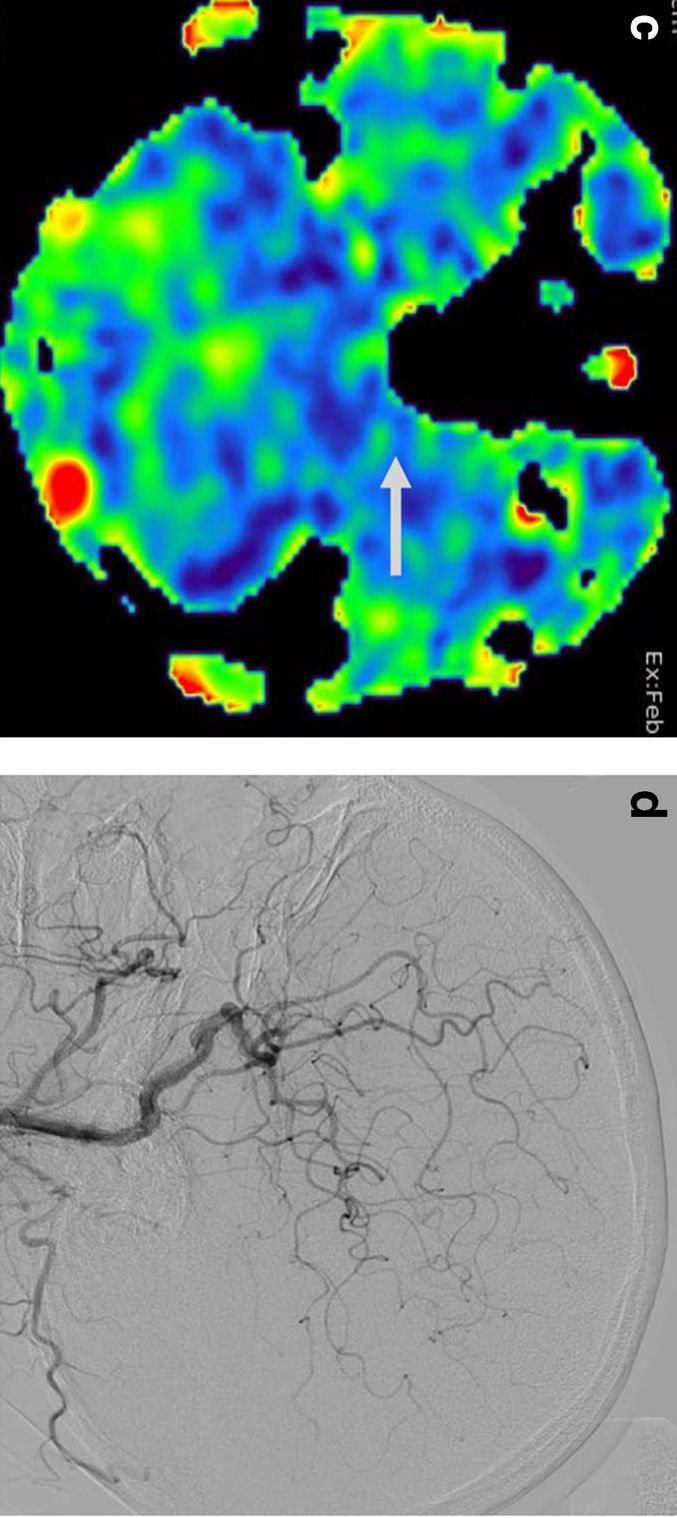
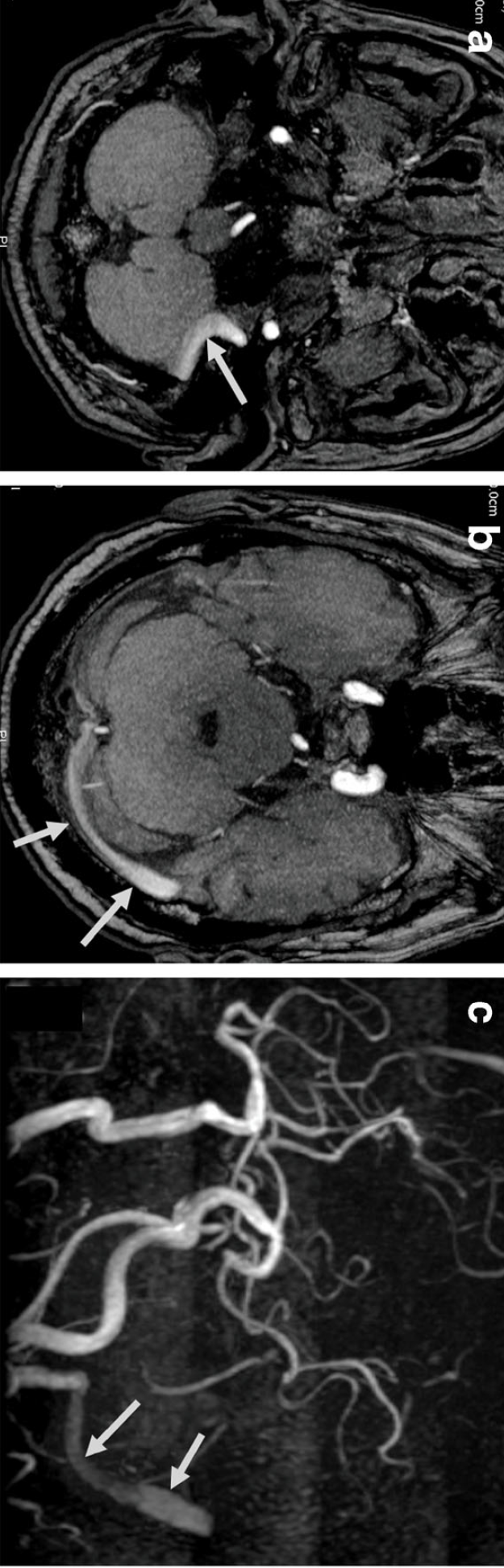
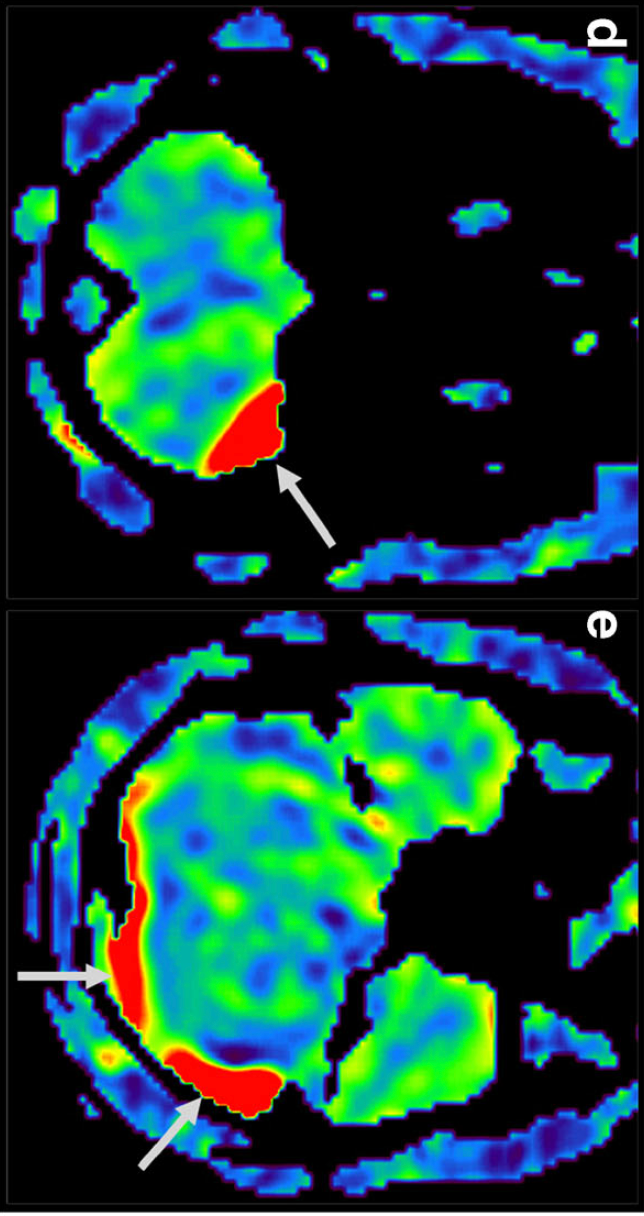
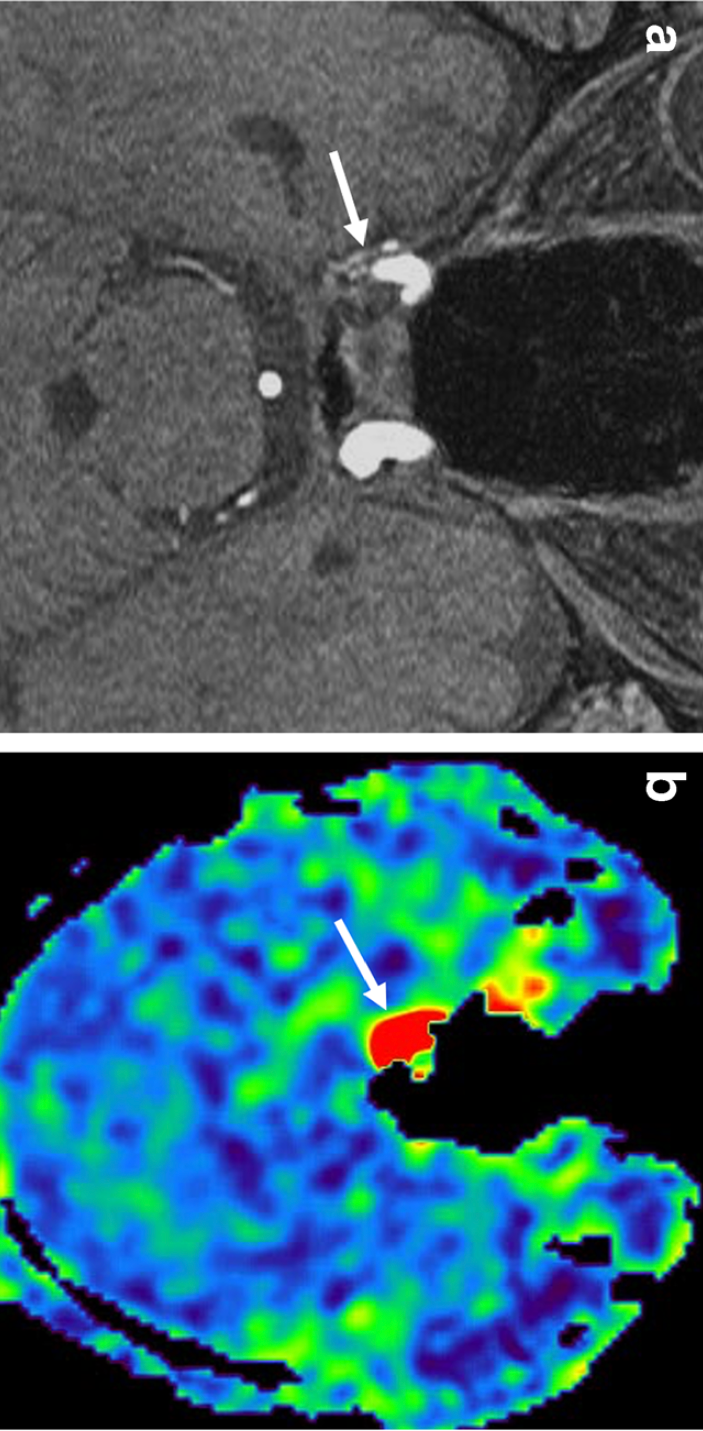
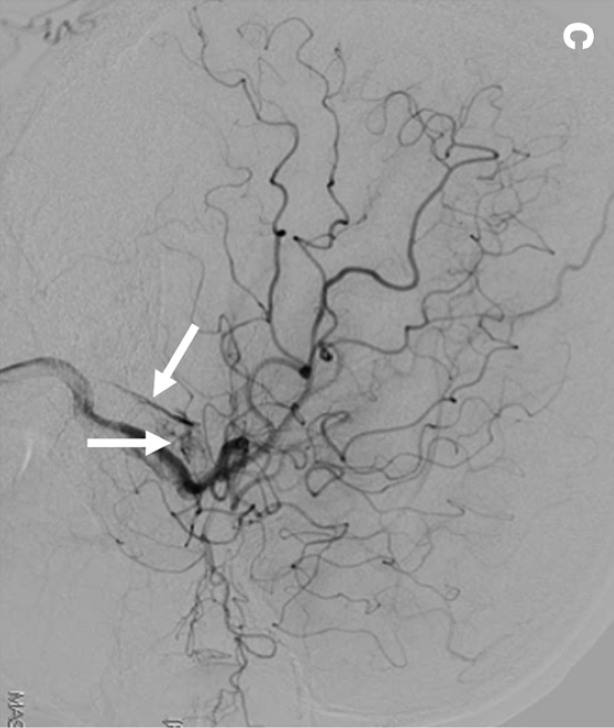
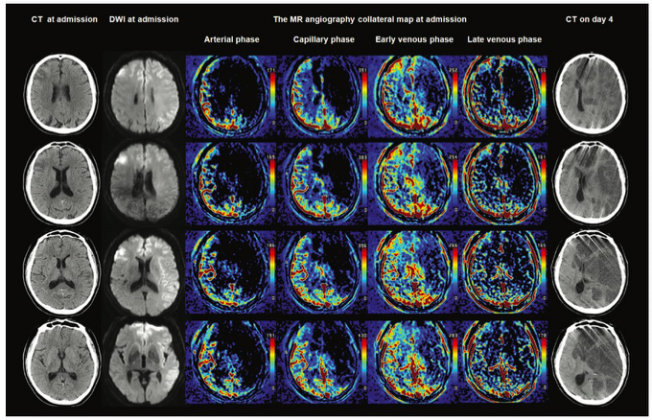
3D TOF MRA是一种无创性成像技术,广泛应用于各种脑血管疾病的MRI检查中。MRA还可用于筛查乙状窦(sigmoid sinus,SS)、横窦(transverse sinus,TS)、海绵窦(cavernous sinuses,CS)等的硬脑膜动静脉瘘(dural arteriovenous fistula,DAVF)。海绵窦DAVF的MRA特征通常指可见到静脉结构,如海绵窦、岩下窦(IPS)、岩上窦、翼丛(PP)、大脑中浅静脉、眼上静脉和蝶窦。 在3T MRA上经常可以看到逆向血流的高信号。先前的研究发现,在406名健康受试者中,43名(10.6%)受试者MRA的海绵窦上可见高信号。这些高信号被认为是翼丛/导静脉(EV)的反向血流信号,如来自颈内静脉(IJV)和乙状窦的反向血流。尽管以前的研究者描述了MRA海绵窦上偶见高信号的病理学和非病理学影像特征,但很难区分这个高信号是因为反向血流还是隐匿性海绵窦 DAVF。 图示1:翼丛(Pterygoid plexus,PP)/导静脉(Emissary vein,EV)的5点分级:I级=PP/EV的部分血流信号(箭头)高于背景信号,低于动脉信号;II级=PP/EV的部分血流信号(箭头)等于动脉信号;III级= 高信号(箭头)区域<=1/3海绵窦区域;IV级=高信号(箭头)区域>1/3海绵窦区域: 图示2:岩下窦(Inferior petrosal sinus,IPS)和海绵窦(Cavernous sinuses,CS)的5点分级:I级=部分IPS的血流信号(箭头)高于背景信号,低于动脉信号;Ⅱ级=部分IPS的血流信号(箭头)等于动脉信号;III级=高信号(箭头)区域<=1/3海绵窦区域;IV级=高信号(箭头)区域>1/3海绵窦区域: 示例1:72岁,男性,PP/EV 分级为 IV 级。MRA 原始图像(a)和 MIP(b)显示左侧 PP/EV 和海绵窦高信号(箭头)。ASL(c)未见PP/EV 和海绵窦高信号(箭头)。DSA 未见海绵窦 DAVF(d): 示例2:72岁,男性,无 DAVF。MRA 原始图像(a,b)和 MIP(c)可见左侧横窦和颈内静脉(箭头)高信号。ASL 显示左侧横窦和颈内静脉(箭头)高信号。这种高信号来源于反向血流(译者注:不是 DAVF,未提供 DSA): 示例3:67岁,男性,右侧海绵窦 DAVF(Cognard I)。MRA 原始图像(a)显示右侧海绵窦轻微升高的信号(箭头)。ASL(b)显示右侧海绵窦高信号(箭头)。DSA 显示右侧海绵窦 DAVF(c): 2021年6月来自日本的Shingo Kakeda等在Neuroradiology上报道了364例(728侧)无动静脉分流患者的 MRA,在 MRA 上发现99侧(13.6%)可见海绵窦反向血流高信号,而没有一例的 ASL 表现高信号。在这些病例中,3侧乙状窦、3侧横窦和8侧颈内静脉高信号。所有这些MRA上静脉窦的高信号都是因为反向血流。 最终作者认为,对于鉴别反向静脉血流和海绵窦 DAVF,ASL 是一种简便易行和有用处的 MRI 序列。对于乙状窦和横窦,由于来自于颈静脉的反向血流,ASL 会产生假阳性的结果,这是 ASL 的局限性,影像学专家应该警惕这种 ASL 的局限性。 译者注:这篇文章的意思是说,MRA 上海绵窦高信号不少见,大部分都是因为反向静脉血流所致。如果 ASL 阴性(绝大部分都是 ASL 阴性),提示反向血流;如果 ASL 阳性可能是由于反向血流所致,也可能是 DAVF。 文献出处: Neuroradiology. 2021 Jun;63(6):889-896. doi: 10.1007/s00234-020-02588-5. Epub 2020 Oct 21. High-signal venous sinuses on MR angiography: discrimination between reversal of venous flow and arteriovenous shunting using arterial spin labeling 图文来源|脑血管病及重症文献导读 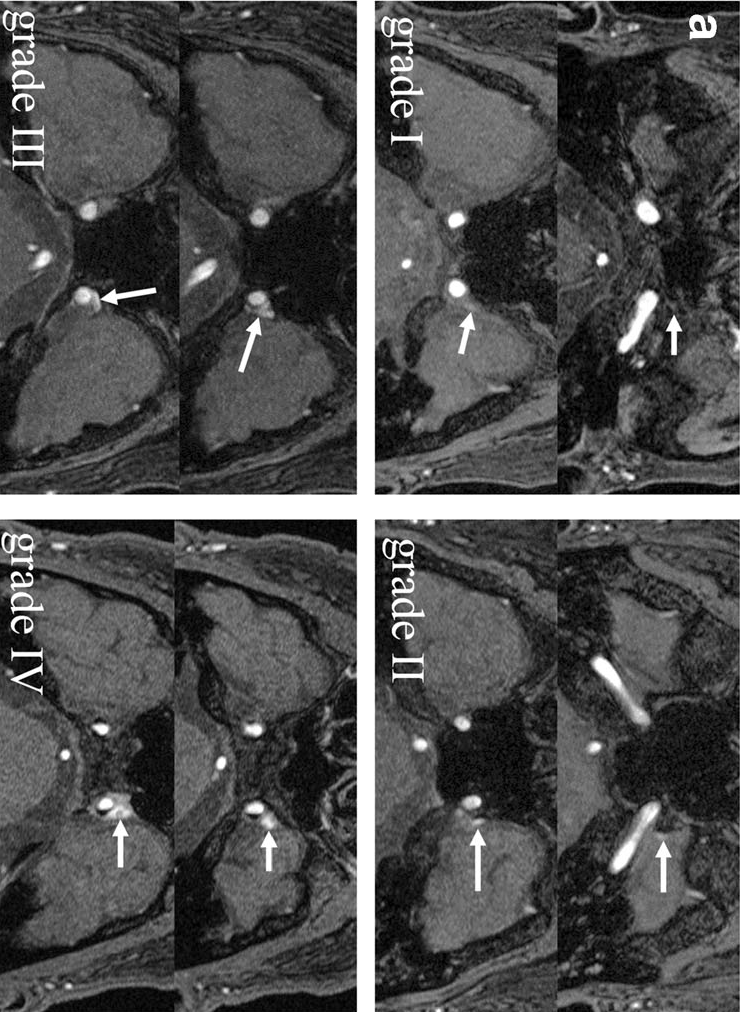

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#静脉#
26
#高信号#
32
#MRA#
41
#静脉窦#
28