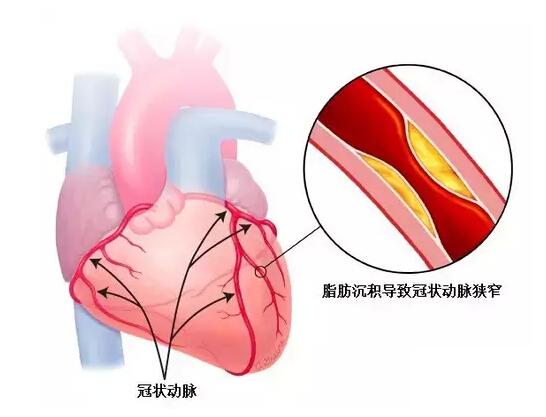
Heart:稳定型心绞痛患者应使用心脏CT还是运动负荷试验?
2016-01-17 QQduhp 译 MedSci原创
目的该研究的目的是评估稳定性心绞痛患者进行心脏CT和运动负荷试验(EST)对患者健康相关性生活质量的改善对比。 方法研究人员在北爱尔兰进行随机对照试验,并采用成本效益分析方法评估。稳定性心绞痛患者随机接受心脏CT检查或EST检查。关注的主要结果是患者每一质量调整生命年(QALY)的医疗花费情况。 结果一共有500名患者参与实验,研究人员随机分配参与者接受心脏CT检查或EST检查,两组人数相等。结果
原始出处:
,A M Agus, P McKavanagh, et al,The cost-effectiveness of cardiac computed tomography for patients with stable chest painHeart,14,Jan,2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#稳定型#
29
#心脏CT#
32
学知识
156
#ART#
30
#HEART#
24
#稳定型心绞痛#
21
赞一个
119
关注
106