JCEM:糖化血红蛋白水平与酸相关上消化道疾病发生率的关联
2022-02-12 MedSci原创 MedSci原创
较高的糖化血红蛋白水平与较高的酸相关上消化道内镜异常风险相关。努力更好地控制血糖可能有助于预防晚期胃肠道并发症的发生率。
随着患病率和相关发病率的增加,糖尿病已成为全球公共卫生的主要问题。糖尿病与胃肠道 并发症有关,包括胃食管反流病(GERD)、胃轻瘫、腹泻和便秘等。先前的横断面研究表明,糖尿病和较高的糖化血红蛋白水平与较高的消化道并发症发生率相关。然而,血糖状态是否与酸相关的上消化道疾病相关仍未明确。

近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,研究人员分析了于2005年到2011年期间在台大医院进行过多次上内镜检查的连续就诊的受试者。
酸相关内镜异常被定义为糜烂性食管炎(EE)、巴雷特食管(BE)和消化性溃疡疾病(PUD),包括胃溃疡(GU)和十二指肠溃疡(DU)。所有受试者均按糖化血红蛋白水平的三个三分位数进行分类。研究人员分析了随访期间各种酸相关疾病的发生情况。
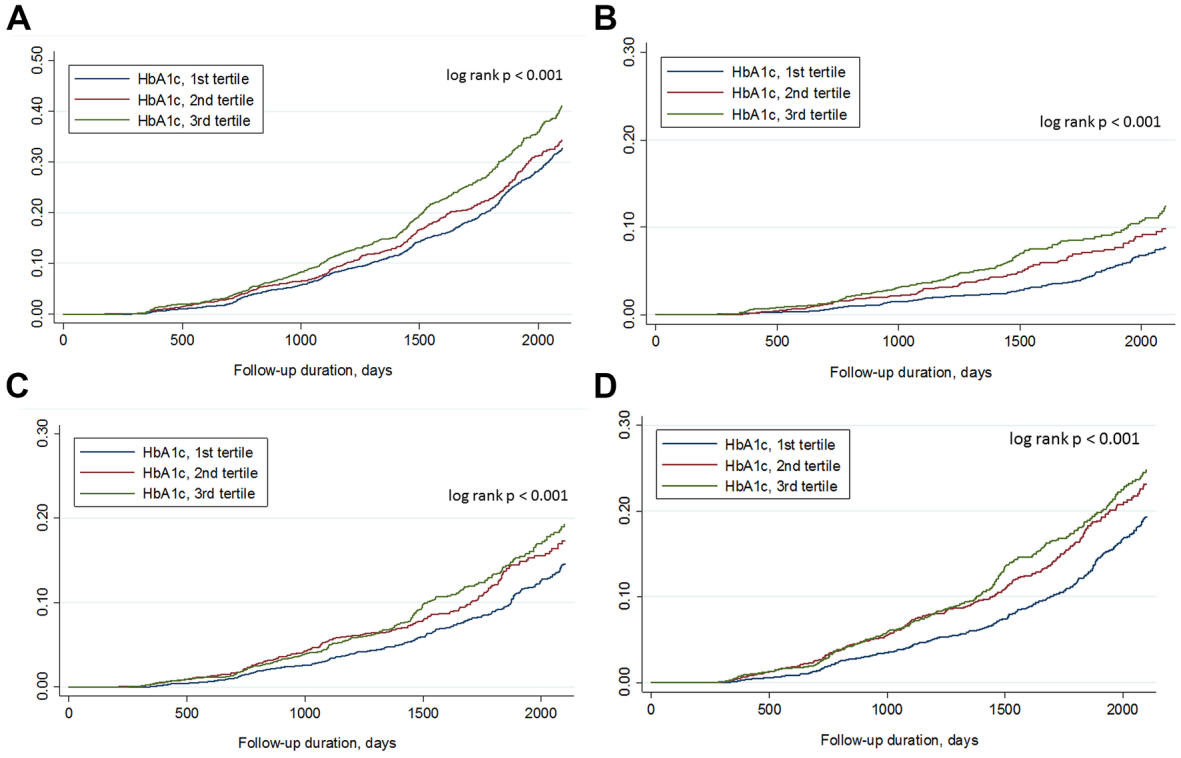
该研究共有11391名参与者(平均糖化血红蛋白水平为5.6±0.7%)参加了纵向随访。在38426.3人次每年的随访中[平均持续时间为3.37±1.59年],EE、BE、GU、DU、PUD和任何酸相关疾病的发生率分别为22.1%、0.5%、4.5%、8.6%、12.3%和30.3%。在随访期间,较高的糖化血红蛋白水平与较高的疾病事件风险相关,除了BE(所有对数秩p<0.001)。在完全调整混杂因素的Cox回归分析中,对于糖化血红蛋白水平处于第三个三分位数的个体,EE、GU、DU、PUD和酸相关疾病的风险比分别为1.174、1.339、1.24、1.24和1.186(所有p<0.05)。
由此可见,较高的糖化血红蛋白水平与较高的酸相关上消化道内镜异常风险相关。努力更好地控制血糖可能有助于预防晚期胃肠道并发症的发生率。
原始出处:
Ping-Huei Tseng.et al.Association of incidence of acid-related upper gastrointestinal disorders with glycated hemoglobin level.JCEM.2022.https://academic.oup.com/jcem/advance-article-abstract/doi/10.1210/clinem/dgac062/6521241?redirectedFrom=fulltext&login=false
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JCE#
37
#JCEM#
34
#发生率#
33
#上消化道#
50
#消化道#
34