一例罕见致病菌导致的感染性心内膜炎的诊疗过程
2021-12-13 潘宏伟等 山东大学齐鲁医院 “检验医学”公众号
感染性心内膜炎是病原微生物经血液侵及心内膜、心脏瓣膜及心脏缺损等处,形成瓣膜、腱索或心房室壁内膜的炎症,以赘生物形成、瓣膜进行性损害等为主要特点。
感染性心内膜炎(infectiveendocarditis,IE)是病原微生物经血液侵及心内膜、心脏瓣膜及心脏缺损等处,形成瓣膜、腱索或心房室壁内膜的炎症,以赘生物形成、瓣膜进行性损害等为主要特点。IE是一种发病率较低的疾病,仅为(3~10)/10万人×年,但其死亡率高达30%。虽然诊断和治疗技术不断进步,但是近二十年来IE患者逐年增多,因此IE仍是临床威胁生命的心血管疾病之一。
针对IE患者,临床上主要是明确感染的病原微生物后进行抗感染治疗,抗感染治疗后的IE极易复发,导致治疗时间延长,最终可能需要外科手术清除感染灶才能治愈。临床微生物室准确及时鉴定导致感染发生的病原微生物,给临床提供合理有效的抗生素治疗方案对于IE患者的愈后具有重要意义。本文分享一例罕见致病菌导致的感染性心内膜炎的诊疗过程。
案例经过
患者,男,因反复间断性发热入院。该患者40年前入伍体检时发现心脏瓣膜疾病,未进行进一步诊断,平素无明显症状。10个月前患者出现无明显诱因发热,体温最高达39.6℃,日间夜间无明显规律,伴乏力及呼吸困难,无恶心呕吐、咳嗽咳痰等,持续约4天。当地医院给予青霉素、退热治疗后发热缓解。一周后患者再次出现发热,体温高达39℃以上,持续数天。后患者反复出现上述发热表现,来我院就诊。经门诊彩超检查,以感染性心内膜炎联合瓣膜病变收入我院心外科治疗。
患者入院初期无明显发热,于入院第2天采集血培养送检,在送检的一套血培养瓶中,需氧瓶报阳,经MALDI-TOFMS质谱鉴定为鲍曼不动杆菌。临床反馈该患者无明显发热等症状,对本次培养结果表示怀疑。我们建议临床再次抽取血培养送检,且抽血过程中要严格做好无菌操作。
随后临床在患者入院的第4,5,6天分别抽取血培养送检。培养结果五天后均为阴性。结合后三次血培养结果及患者的临床症状,本次培养获得的鲍曼不动杆菌为污染菌株。经与临床再次沟通,建议患者发热时再行抽血送检,并再次强调抽血中要严格做好无菌操作。
入院后第10天患者出现发热现象,体温为37.6℃,临床给予物理降温的同时留取血培养。后连续三天送检血培养。本次送检血培养均在三天以后报阳:涂片显示革兰氏阴性小杆菌,聚团存在,长短不一(见图1)。我们初步怀疑可能是布鲁氏菌。由于布鲁氏菌具有传染性,二级生物安全实验室最好不要进行该菌株的鉴定,建议临床送检传染病医院进行血清凝集实验。
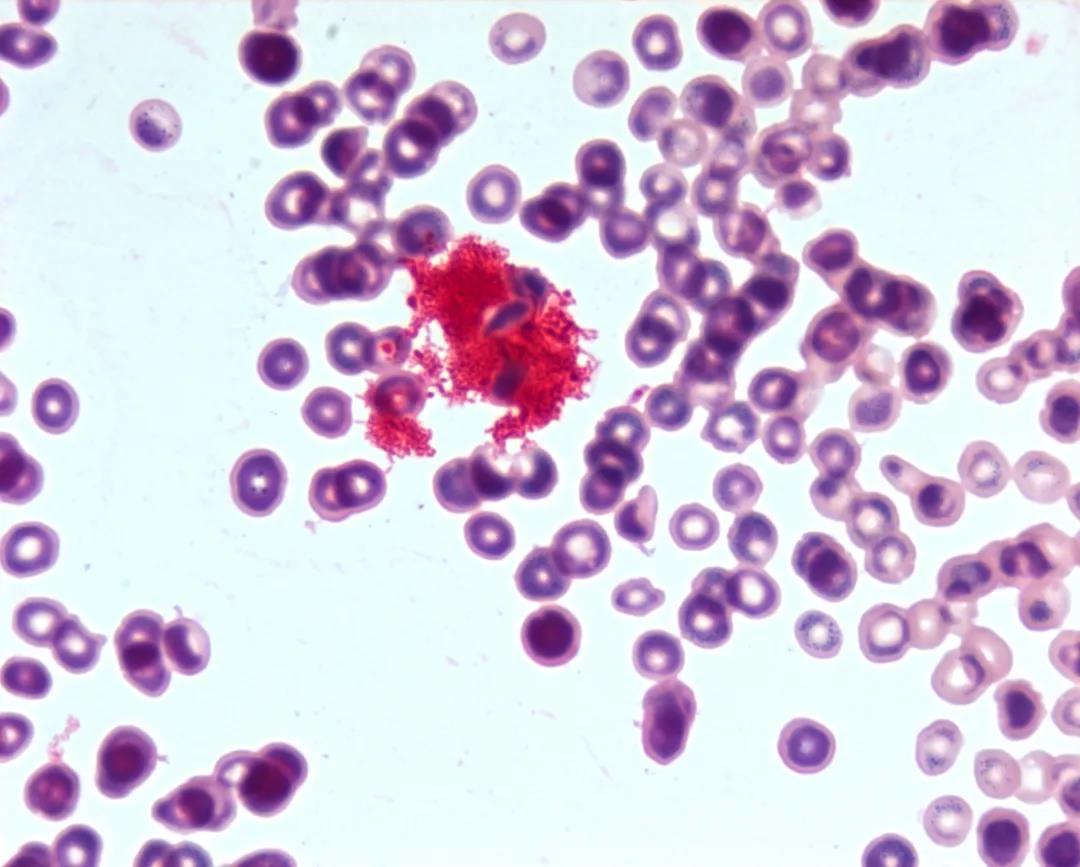
图1 阳性血培养瓶显微镜下菌株形态
布鲁氏菌血清凝集实验为阴性,且患者自述近期无牛羊接触史。需等待实验室进一步的培养鉴定结果。该菌株在血平板上生长极为缓慢,3天后血平板生长出大小不一的菌落克隆,经反复分纯后仍为该菌落形态(见图2)。后针对该菌落进行MALDI-TOFMS 质谱鉴定,未获得鉴定结果。梅里埃Vitek2 鉴定为缺陷短波单胞菌,但可信度较低,且未获得药敏结果。
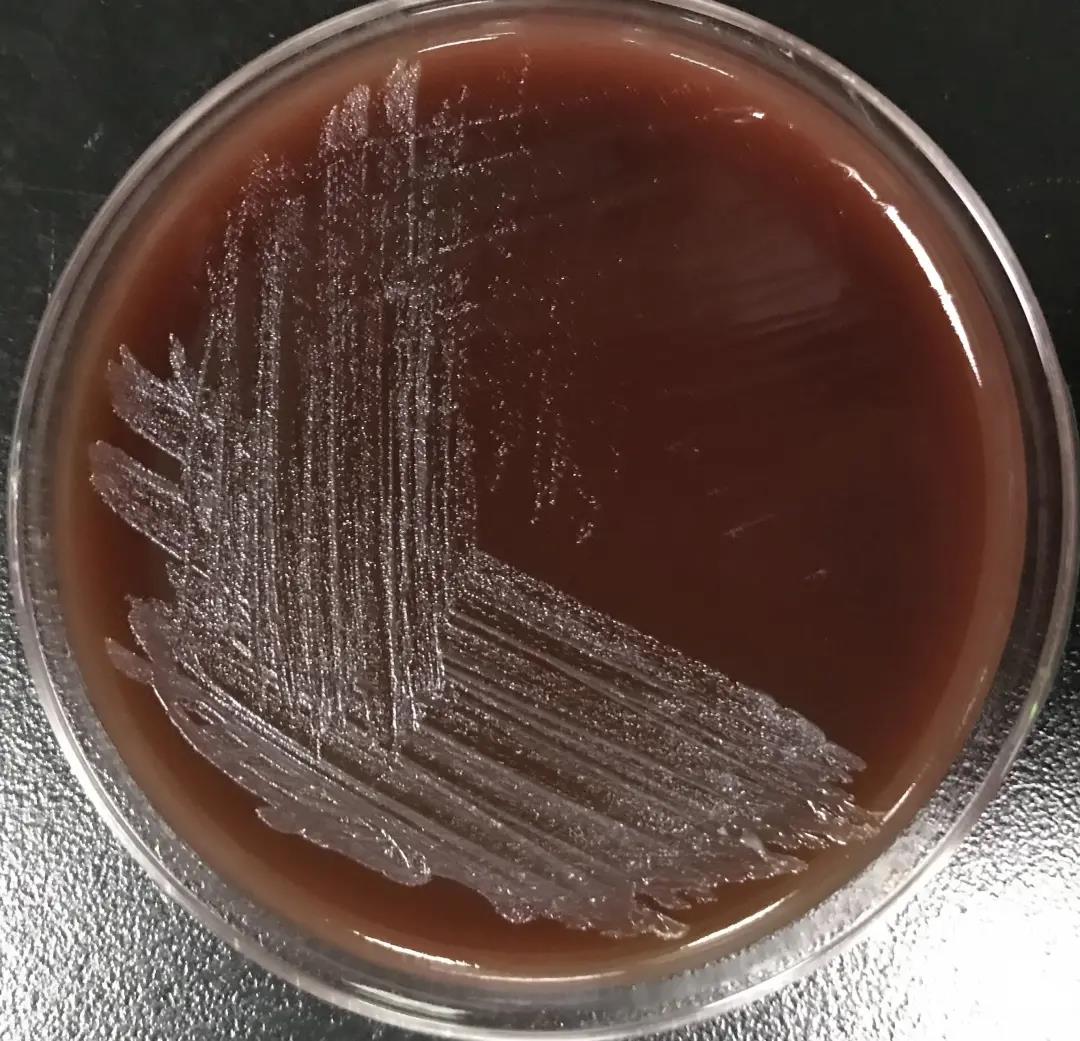

图2 阳性血培养血平板的菌落及显微镜下形态
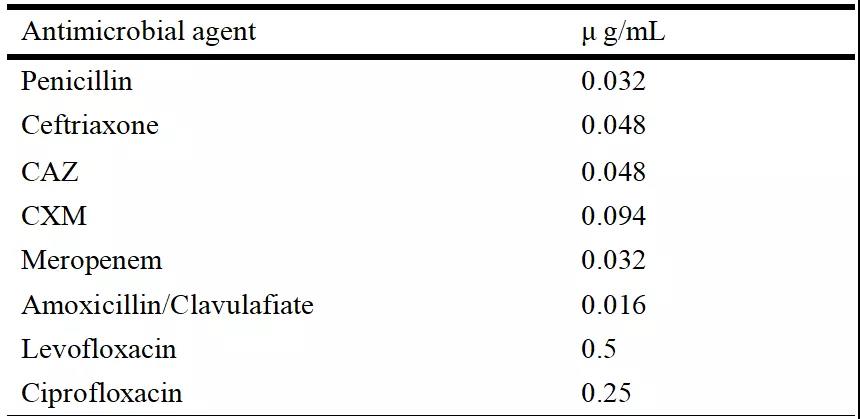
为给临床提供获得准确的鉴定结果及后续药敏结果,我们实验室同时送检该菌株的基因组DNA进行16SrDNA基因组测序鉴定。后鉴定结果为Bergeyella cardium(作者自主翻译为:心内膜炎伯杰氏菌)。根据该菌株的生长特点,随后采用E-test方法,使用血平板对菌株的药敏进行了测试分析。由于该菌株无药敏折点,实验室将MIC分析数值提供临床参考(见表1)。临床选择美罗培南进行抗感染治疗后行手术治疗,术后3周患者血培养阴性,未出现发热现象,后患者痊愈出院。
表1 MIC分析数值
案例分析
心内膜炎患者血培养采集及结果正确判读
血培养为鉴定致感染性心内膜炎发生病原菌的主要方法。针对急性感染性心内膜炎患者建议立即或者抗菌药物治疗前采集血培养2-3套;亚急性心内膜炎患者建议每间隔30分钟-1小时采集一套血培养,不同部位连续采集3套血培养,若24小时培养阴性,宜加做2套血培养。
本案例中的患者属于亚急性心内膜炎患者,入院初期即抽取血培养,初次培养在送检的血培养中仅一需氧瓶报阳,鉴定为鲍曼不动杆菌。虽然鲍曼不动杆菌是常见的临床致病菌,但是该患者在3套血培养中仅有一瓶报阳,且没有该菌感染的临床指征,经实验室和临床医生沟通交流判定为该菌株为污染菌株。
后在患者再次发热时,抽血三套血培养,本次三套血培养均在培养3天左右报阳,初步判定本次阳性病原菌为导致感染性心内膜炎的病原菌。抽取血培养时,正确严格的皮肤消毒和“双瓶双侧”原则对于结果的正确获取至关重要,否则污染菌株极易掩盖真正病原菌,特别是像本案例中的苛养病原菌;双瓶双侧原则也有利于污染菌株的排除,如本案例初次获取的阳性培养菌鲍曼不动杆菌为污染菌的判定。
对于无药敏折点的罕见病原菌,如何选择抗生素治疗?
随着诊疗技术的进步,越来越多的新发和罕见病原菌将被鉴定和发现,而这类病原菌多数无药敏折点。针对本案例中的Bergeyella cardium(作者自主翻译为:心内膜炎伯杰氏菌)无药敏这一难点,我们主要是借助以下方法来助力临床抗生素治疗:
一、查阅文献,看看有没有类似菌株感染的患者的治疗方案。2015年,韩国研究者先后从两例感染性心内膜炎患者中分离到了伯杰氏菌属细菌,上述两位患者均使用青霉素进行治疗。但本案例中患者在地方医院时使用青霉素治疗是失败的,因此无法借鉴上述治疗方案。
二、利用三代测序技术,分析了该菌株中的耐药基因,发现其对氟奎诺酮类药物天然耐药,并将结果提示给临床。
三、与临床沟通后,并根据该菌株的特点,采利用E-test方法,测量了几类主要抗生素进行了MIC值的测定,提供给临床医生作为治疗参考。
知识拓展
常用细菌鉴定方法比较分析
目前对于可培养细菌的鉴定方法主要包括生化反应仪器鉴定法、MALDI-TOFMS质谱鉴定法及16srDNA基因测序鉴定法。生化反应仪器鉴定法是临床微生物室最为常用的鉴定方法,因该鉴定方法存在鉴定时间长、准确率低等不足,目前正逐渐被MALDI-TOFMS质谱鉴定法所取代。
MALDI-TOFMS质谱鉴定法是基于细菌核糖体蛋白质组的菌株鉴定方法,具有快速、准确、易操作等优点。但是其也存在一定不足,如对于蛋白质组图谱接近的细菌无法区分,数据库包含菌株数目具有一定的局限性。16srDNA基因是细菌进化的分子标尺,是鉴定难区分菌株、新发病原菌株或未描述病原菌株的关键技术。
目前,新的病原菌鉴定趋势是将MALDI-TOFMS质谱鉴定法和16srDNA基因测序鉴定法结合起来使用,以达到更好的菌株鉴定。在本案例中,我们在确保质谱鉴定无误的情况下仍无法获得鉴定结果,推测该菌株可能是质谱数据库外的少见病原菌,因此开展了16srDNA基因测序鉴定,发现了Bergeyella cardium[5](作者自主翻译为:心内膜炎伯杰氏菌)这一罕见致病菌。
伯杰氏菌简介
伯杰氏菌属(Bergeyellasp)是属于黄杆菌科的非发酵革兰氏阴性需氧杆菌。目前其相关研究主要是该属细菌感染导致疾病发生的病例报道。2006年Beltran等人报道了由于食用含有山羊血的食物导致动物溃疡伯杰氏菌感染进而引发菌血症的病例。同年Kallman等人报道了由于动物溃疡伯杰氏菌株感染导致蜂窝组织炎的病例。
在之后的十几年里陆续有多位研究者报道了由于动物溃疡伯杰氏菌感染导致的各类感染性疾病的发生。此外,伯杰氏菌属其他细菌导致感染性疾病发生的病例也被报道。2006年美国研究者Han等人发现来源于口腔中的不可培养的Bergeyellasp. cloneAF14可能是导致早产发生的致病菌。
因此,伯杰氏属细菌的感染可导致菌血症、肺炎、脑膜炎、蜂窝组织炎、脓肿、等疾病的发生,可能是重要的人类条件致病细菌。近年来分离自感染性心内膜炎患者血培养中的伯杰氏属细菌的陆续报道,2015年,韩国研究者先后从两例感染性心内膜炎患者中分离到了伯杰氏菌属细菌,分别被命名为B.cardium 13-07T和B.cardium 13-16 。2017年和2018年我国研究者Chen及Guo等人也先后报道了自感染性心内膜炎患者发现伯杰氏致病菌的病例。
案例总结
本案例介绍了一例由罕见致病菌导致的感染性心内膜炎的诊疗过程。最初不管是生长特性还是显微镜下形态观察其与布鲁氏菌极易混淆,后经过布鲁氏菌血清凝集实验、生化反应鉴定和质谱鉴定排除该菌感染的可能。MALDI-TOFMS质谱鉴定虽然获得较好的肽指纹图谱但是未在数据库中获得比对结果,提示我们该病原菌株可能是新发病原菌株或者是数据库中未包含的罕见病原菌。
随后借助16srDNA基因测序鉴定该菌为Bergeyella cardium(作者自主翻译为:心内膜炎伯杰氏菌),该菌是与感染性心内膜炎相关的罕见致病菌。随着诊疗技术的进步,越来越多的新发和罕见致病菌将被临床微生物室培养获得,期望本案例中病原菌的鉴定及分析过程能为类似病原菌的诊疗提供一定的启示和帮助。
专家点评
规范的微生物标本采集、运送是准确的病原学诊断的前提;及时、准确的微生物检验结果可以为临床感染性疾病的诊断、治疗提供科学依据。
随着实验室检验技术的提高,越来越多的新发和罕见致病菌将被发现,这将对实验室和临床治疗带来新的挑战!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#内膜#
41
#感染性#
32
#心内膜炎#
56
#罕见#
44
#致病菌#
43
深刻体会到了
59
学习呢
63
学习了
71