Neurology:儿童非意外创伤所致脊髓硬膜下血肿
2019-08-12 zyx整理 神经科病例撷英拾粹
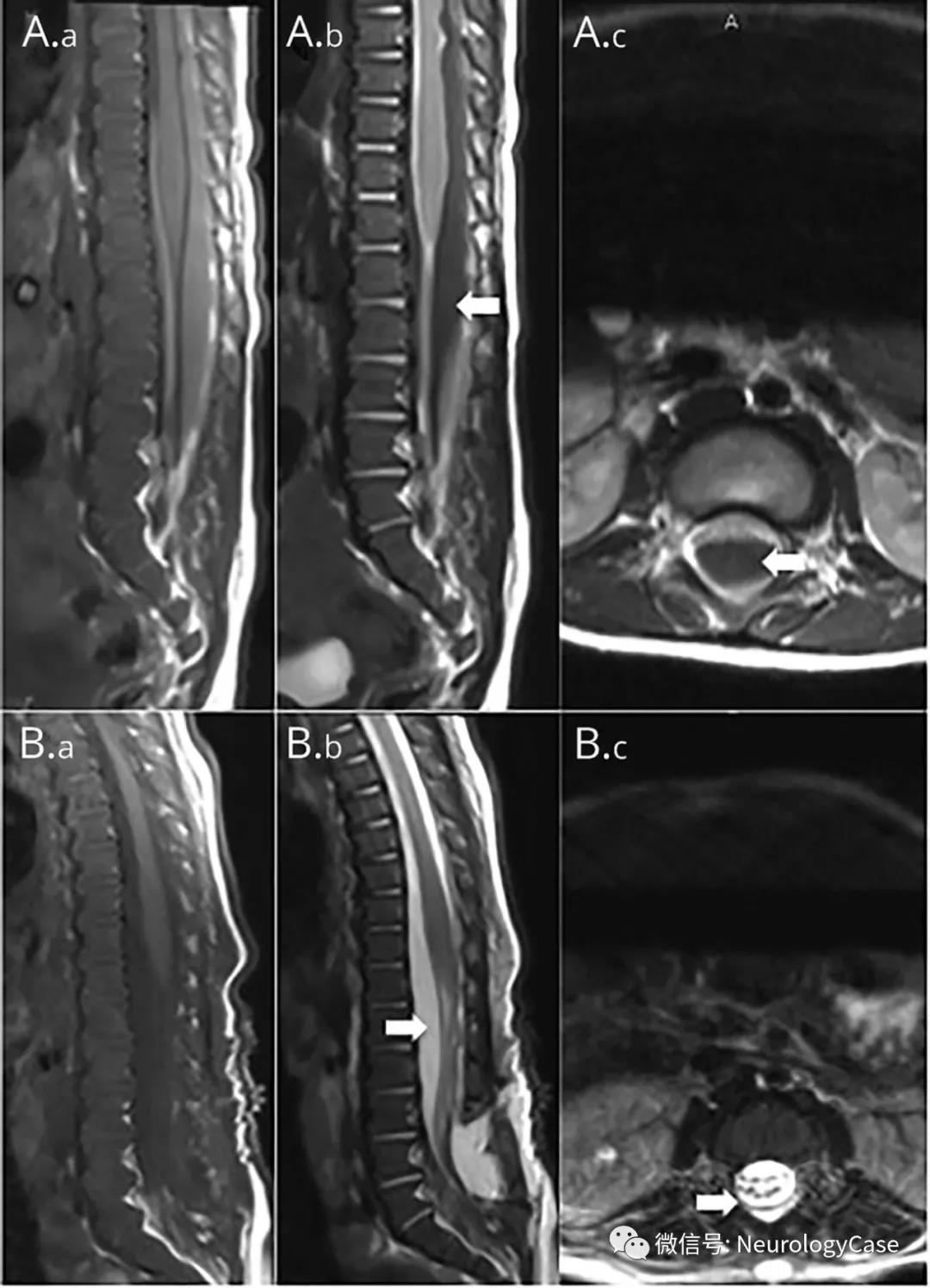
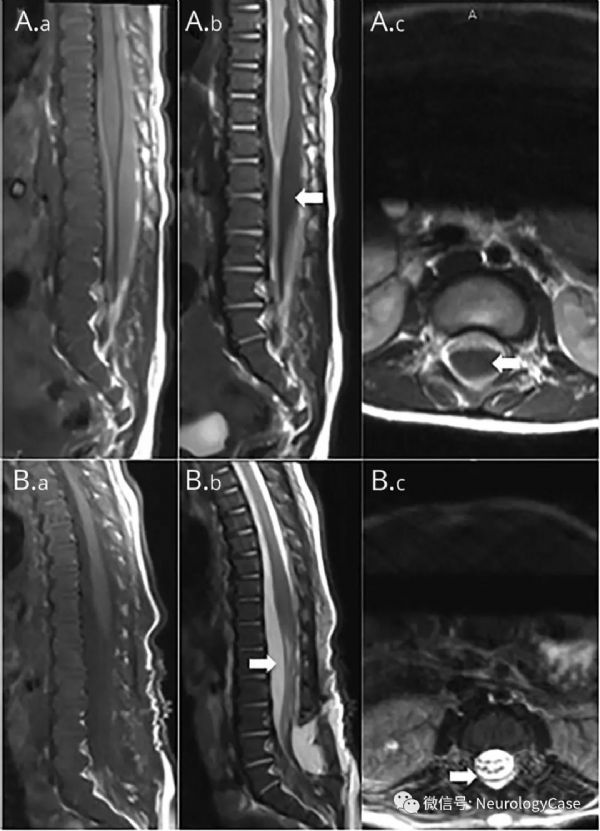
5月大男孩,非意外创伤致双侧颅内硬膜下血肿,神经系统查体配合欠佳,仅可见肢体退缩反射。脊柱成像(图)可见横跨T4-L5的硬脊膜下血肿伴脊髓受压。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Neurol#
0
#硬膜下#
29
#创伤#
25
#血肿#
40
#硬膜下血肿#
0
学习了
74