Stroke:颈动脉夹层串联病变的机械取栓
2017-12-13 杨中华 脑血管病及重症文献导读
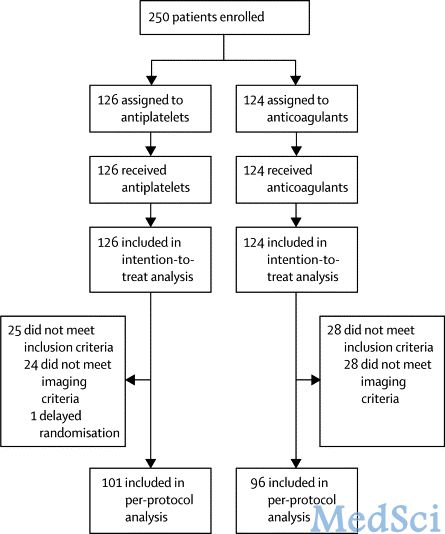
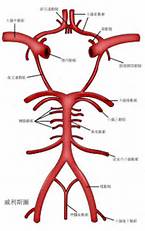
从技术上来讲,前循环串联病变采用血管内血栓切除术是一项挑战,但是HERMES工作组发现串联病变和孤立性颅内闭塞的预后类似。颈总动脉狭窄-闭塞的2个重要的病因为动脉粥样硬化和动脉夹层,这两项病因对血管内治疗后再灌注和临床预后的影响尚不清楚。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#颈动脉#
38
#颈动脉夹层#
46
#取栓#
42
#动脉夹层#
42
#机械取栓#
43