山东学者:诊断冠脉重构,这种冠脉CT能大显身手
2019-08-29 宋达琳,徐余鸣,马千里,等 中国循环杂志
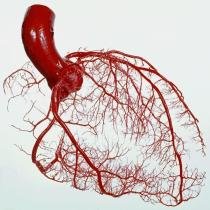
血管内超声是诊断冠脉重构的金标准,但有创且贵,Gemstone 能谱冠状动脉 CT 血管成像(CCTA)无创、辐射低、安全性高,而且图靓性价比高,诊断冠脉重构价值高不高?
山东省青岛市市立医院张庆、宋达琳等进行的研究显示,Gemstone 能谱 CCTA 能精确测量与重构性质相关的各种参数,反映斑块负荷从20% 到80%不同分组的冠脉重构变化。
冠脉重构是动脉粥样斑块与管腔之间复杂关系的重要现象,在斑块形成早期,当斑块负荷在 20% 以下时,外弹力膜扩张发生正性重构,管腔不会发生狭窄。
当斑块负荷继续增加但未超过40% 时,外弹力膜无法进一步扩张,管腔开始缩小;当斑块负荷增加到 40% 以上时,外弹力膜开始皱缩,发展为负性重构,加重管腔狭窄。
研究显示,冠脉正性重构和无重构的患者,病变处外弹力膜直径明显大于负性重构患者,无重构患者近端参考段外弹力膜直径均明显大于正性重构和负性重构患者。
研究还发现,病变处外弹力膜直径、病变管腔直径在不同斑块负荷的患者中差异较为显着,除斑块负荷>80% 的患者外,斑块负荷在20%~80%变化时,病变处外弹力膜直径和管腔直径都随斑块负荷增加而降低。
不过研究未发现,通过重构指数计算的正性重构和负性重构之间未显示斑块负荷的差异。
诸多血管内超声及病理学研究发现大部分不稳定性心绞痛患者表现为正性重构,大多数稳定性心绞痛患者则表现为负性重构,冠状动脉斑块破裂更容易发生在正性重构的病变部位。
研究者指出,尽管血管内超声对冠脉斑块性质、重构类型判断有其优势,但 Gemstone 能谱 CT 的无创性、可以提供精准解剖定位、精准重构类型诊断,能够优势互补。
研究者认为,CCTA 是多模态影像学对冠脉重构类型诊断研究的重要组成,对个性化精准医疗有重要意义。
该研究共纳入76例冠心病患者,平均63.9岁,均存在左主干或左前降支近段病变。研究者选取了这两段冠脉进行了研究。
根据重构指数(RI)分为正性重构组(RI>1.05)44 例,无重构组(RI 0.95~1.05)21 例,负性重构组(RI<0.95)11 例;又根据斑块负荷,分为斑块负荷 21%~40% 组 30 例、41%~60% 组 30 例、61%~80% 组 14 例和>80%组2例。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#冠脉重构#
33
#冠脉CT#
35
好好好好好好
70
学习
75
好
75