多灶性白质脑病如何治疗?NT-I7(efineptakin alfa)将进入临床试验阶段
2021-02-24 Allan MedSci原创
NT-I7(efineptakin alfa)是一种新型的长效人类白介素-7(IL-7)。
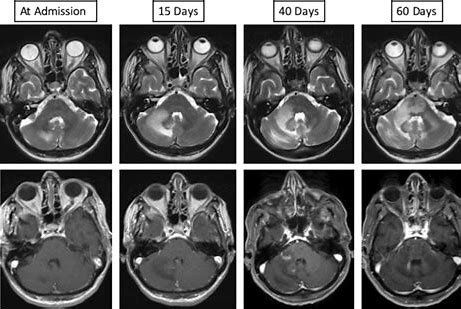
进行性多灶性白质脑病(progressive multifocal leukoencephalopathy, PML)是一种中枢神经系统严重脱髓鞘疾病。PML由多瘤病毒属中的JC病毒再激活所致。儿童期可发生无症状的JCV初次感染,86%的成人中可检出抗体。大多数情况下,JCV主要潜伏在肾脏和淋巴器官中,但出现严重细胞免疫抑制时,JCV会被再激活。
生物制药公司NeoImmuneTech今天宣布,美国食品药品监督管理局(FDA)已批准其研究性试验申请(IND),用于评估该公司的主要候选药物NT-I7(efineptakin alfa)治疗进行性多灶性白质脑病(PML)的有效性和安全性。NT-I7(efineptakin alfa)是一种新型的长效人类白介素-7(IL-7)。
目前,尚无治疗PML的方法,患者存活的唯一可能性是恢复抗病毒免疫反应。因而,促进和加速免疫重建的策略则是抗PML的关键。
NeoImmuneTech首席医学官NgocDiep Le博士说:“继2020年6月NT-I7的FDA孤儿药指定后,IND的获批是NT-I7的又一里程碑。PML主要影响免疫功能低下的个体,我们相信NT-I7可以增强免疫系统的恢复,增强PML患者的免疫反应”。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#多灶性#
40
#脑病#
36
#ALF#
0
#白质#
31
学习了
47
#AKI#
43