JCC: IL-6缺失会加剧IL-10缺乏小鼠的结肠炎并诱发全身性炎症反应
2020-07-12 MedSci原创 MedSci原创
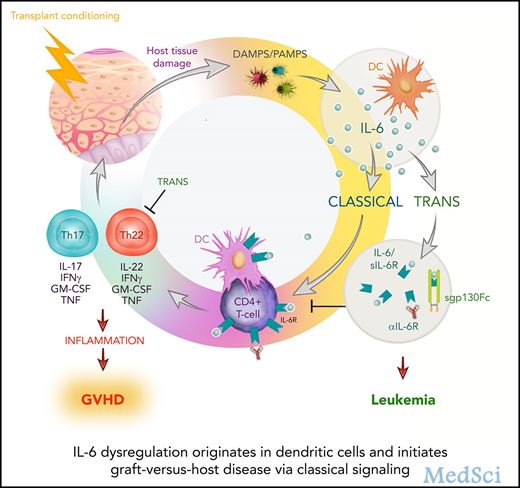
白介素6 [IL-6]或其受体目前是炎症性肠病[IBD]靶向生物治疗的候选目标。
背景和目标
白介素6 [IL-6]或其受体目前是炎症性肠病[IBD]靶向生物治疗的候选目标。因此,必须全面了解阻断IL-6的效果。本项研究旨在通过评估IL-6缺失对IL-10-缺陷小鼠[IL-10 -/- ] 自发性结肠炎的影响进行了探究。
方法
研究人员将产生IL-6 / IL-10双缺陷[IL-6 -/- / IL-10 -/- ]小鼠与野生型相比结肠粘膜的肠道炎症。
结果
出乎意料的是,IL-6 -/- / IL-10 -/-小鼠表现出比IL-10 -/-小鼠更明显的肠道炎症和更早的疾病发作,无论是局部[结肠和小肠]还是全身性[脾肿大,溃疡性皮炎] ,白细胞增多,中性粒细胞增多和单核细胞增多]。IL-6 -/- / IL-10 -/-小鼠表现出多种细胞因子[IL-1β,IL-4,IL-12,TNFα]和趋化因子[MCP-1和MIG]的升高,但IFN-γ没有升高。
结论
在IL-10 -/-小鼠可以部分通过抑制Treg / CTLA-4并促进IL-1β/ Th2途径,完全IL-6阻断可显着加重肠道炎症。另外,双重突变体表现出严重的全身性炎症的迹象。
原始出处:
Mei Ye. Et al. Deletion of IL-6 Exacerbates Colitis and Induces Systemic Inflammation in IL-10-Deficient Mice. Journal of Crohn's and Colitis. 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#IL-6#
33
#炎症反应#
30
#IL-1#
36
#IL-10#
46