JNER:用于楼梯和地面训练的可穿戴踝关节机器人对亚急性中风的影响:一项随机对照试验
2021-09-18 MedSci原创 MedSci原创
中风是导致长期残疾的主要原因。中风患者通常会出现脚部下垂的问题,跌倒的风险很高,因为下垂脚会拖在地面上,很容易被障碍物绊倒。有效的步态恢复对于提高中风幸存者的生活质量和独立性至关重要。亚急性期的早期康
中风是导致长期残疾的主要原因。中风患者通常会出现脚部下垂的问题,跌倒的风险很高,因为下垂脚会拖在地面上,很容易被障碍物绊倒。步态恢复对于提高中风幸存者的生活质量至关重要。亚急性期的早期康复更为有效,但在完成常规步态康复后,约50–60%的中风幸存者仍有一定程度的运动障碍。常规步态康复通常涉及重复和特定任务的步态练习。研究表明,在亚急性和慢性中风中,楼梯上的强化步行训练可以提高步行速度和平衡。

亚急性中风幸存者参与早期步态训练,并使用机电辅助机器人,如Lokomat、步态训练器和G-EO系统,可以在一定程度上改善步态独立性的恢复。但是这些步态训练系统将使用者限制在像跑步机一样的固定环境中。步态康复的一个重要目标是使独立行走和信心能够在没有护理人员帮助的情况下尽快提高他们的生活质,楼梯的早期中风康复可能会加强步态训练效果,从而在出院时获得更好的步态结果。然而,因为楼梯环境的安全问题楼梯训练并不是亚急性中风的常见临床实践。可穿戴式踝关节机器人可能是一种可行的解决方案,能够在楼梯训练期间更好地控制踝关节。
本研究团队已经开发出一种外骨骼踝关节机器人,用于对患有慢性中风和足部下垂问题的人进行步态训练。该机器人可以提供主动辅助力矩,以促进轻瘫患者踝关节背屈以迈上楼梯,并协助足底弯曲以响应负载(动力辅助模式)。本研究的主要目的是评估可穿戴机器人辅助AFO对亚急性中风幸存者的影响。本文发表在《Journal of NeuroEngineering and Rehabilitation》.

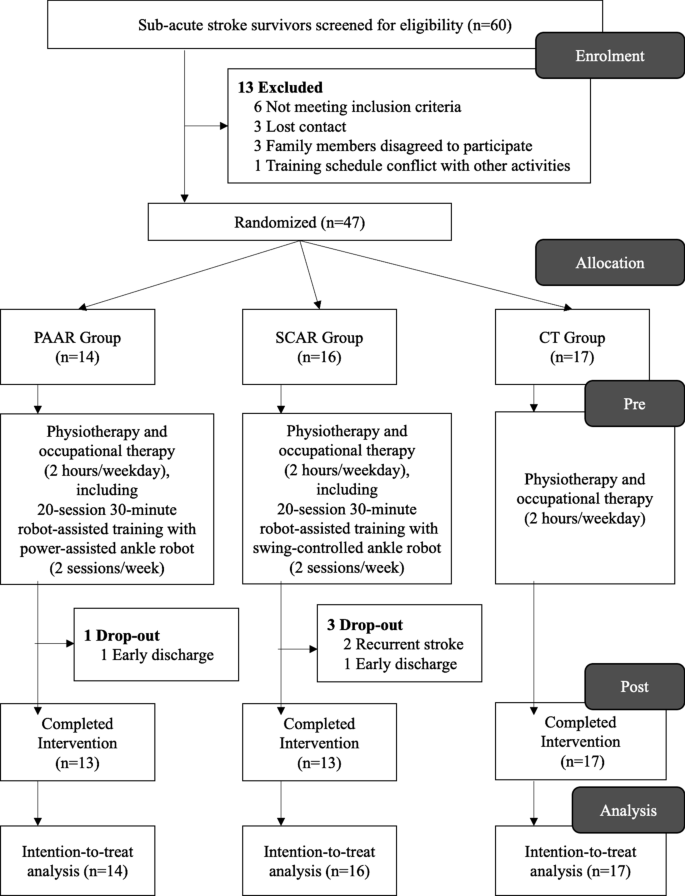
招募的受试者符合以下入选标准,包括2个月内首次发作的中风;单侧缺血性或出血性中风导致的偏瘫;有足够的认知能力来遵循说明并理解研究的内容和目的。招募的受试者通过抽签随机分为三组:(1)动力辅助踝关节机器人(PAAR),(2)摆动控制踝关节机器人(SCAR),(3)常规训练(CT)。所有受试者接受住院训练中心康复团队规定的常规康复方案(物理治疗和职业治疗),时间为2小时/工作日,包括站立、平衡、步进和行走的标准下肢训练。
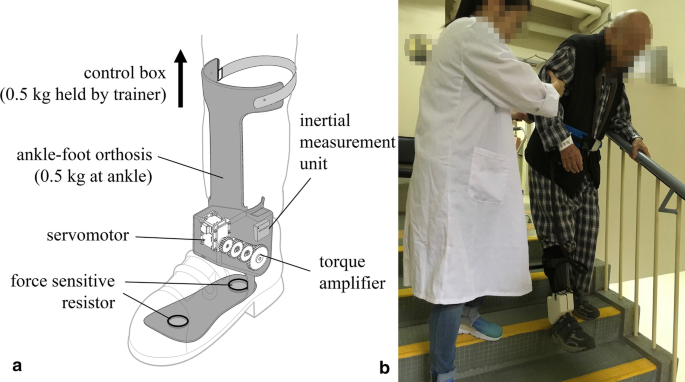
踝部机器人与训练场景
对于分配到PAAR和SCAR的受试者,每天进行30分钟的机器人辅助训练(每周至少两次,总共20次)。每个机器人辅助训练课程包括10分钟的地面行走,然后是10分钟的楼梯训练(上升/下降),然后是10分钟的地面行走。一名医生走在受试者受影响一侧的旁边,并始终握住受试者的腰带以确保安全。受试者使用医院康复团队规定的助行器,包括手杖、四足杖和助行器。康复团队在每次治疗前检查受试者的生命体征并检查其功能能力。医生定期询问受试者在培训期间是否感到疼痛和不适。每次训练都记录了楼梯数量和步行距离,作为训练强度和能力的记录。
PAAR和SCAR均配备有相同的外骨骼踝关节机器人,但操作模式不同,可由医生进行调节。在每个机器人辅助训练课程中,机器人都穿着受试瘫痪一侧的鞋内。该可穿戴机器人由关节式AFO改装而成,可在踝关节背屈/跖屈方向提供动力辅助。该机器人可以通过在脚跟和前掌下放置嵌入式力敏电阻器识别足部负荷和步态阶段的变化。安装在小腿上的惯性测量装置可以测量腿部倾斜角度,以记录用户在水平和楼梯上的行走意图。PAAR模式下的踝关节机器人旨在提供动力踝关节辅助以及剩余运动功能,以促进地面行走和楼梯训练。SCAR模式下的踝关节机器人充当摆动控制矫形器,根据步态阶段在锁定和解锁踝关节之间切换。
实验流程
在训练前和训练后一周内,同一名评估员对受试者进行前后评估。所有评估员都不知道分组分配。所有临床评分均在未使用任何辅助设备的情况下对受试者进行评估,不佩戴任何踝关节机器人和任何矫形器 。主要结果测量是FAC,次要观察指标包括伯格平衡量表(BBS)和定时10米步行测试(10MWT)。
来自两家参与医院的共60名亚急性中风幸存者接受了资格筛查。符合资格标准的中风幸存者被随机分配到PAAR(n = 14) , SCAR(n= 16) ,及CT(n = 17) 。总共有4名中风幸存者没有完成20个疗程(1个PAAR和3个SCAR)。所有退出的受试者在出院前至少完成了10个疗程。未报告严重不良事件或重大损害。 当在机器人辅助训练中佩戴机器人时,PAAR提供的更多主动力辅助可以促进受试者在爬楼梯和地面行走时比SCAR走得更高的节奏和速度。在20次训练中,两组的步频和速度均显著提高(p < 0.001),但PAAR受试者步行速度明显加快。
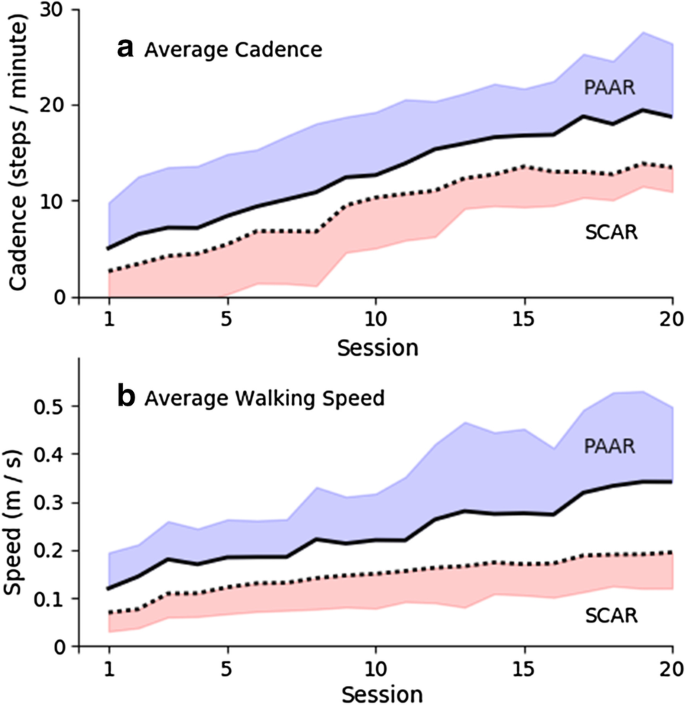
20次机器人辅助训练的训练强度
20个疗程后,PAAR、SCAR和CT在步态独立性(FAC)、平衡性(BBS)和步行速度(10MWT)方面有显著的组内功能改善。组间比较表明,机器人辅助训练(PAAR和SCAR)比常规护理(CT)中的常规训练能显著改善运动功能。组间FAC比较显示,机器人辅助训练和常规训练的效果大小中等(PAAR与CT 0.671,SCAR与CT 0.610)。这表明更大的样本量可能会产生更显著的统计效应。PAAR和SCAR之间的效应大小差异在FAC中较小(0.010),但4周的干预显示10MWT中的效应大小差异较大(0.752),BBS中的效应大小差异中等(0.567)。因此,PAAR可能比SCAR更有利于步行速度和平衡的功能改善。
本文研究结果证明了使用踝关节机器人进行强化楼梯训练用于中风康复的可行性。
Yeung, LF., Lau, C.C.Y., Lai, C.W.K. et al. Effects of wearable ankle robotics for stair and over-ground training on sub-acute stroke: a randomized controlled trial. J NeuroEngineering Rehabil 18, 19 (2021). https://doi.org/10.1186/s12984-021-00814-6
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#对照试验#
35
#对照#
32
#随机对照试验#
33
#机器人#
32
#踝关节#
42
#机器#
26
收获满满
53