Gastroenterology:溃疡性结肠炎激素无应答:肠外甲氨蝶呤是否有效?
2018-11-22 佚名 环球医学
发表于《Gastroenterology》上的一项研究表明,对糖皮质激素无应答或缓解的溃疡性结肠炎(UC),肠外甲氨蝶呤不优于安慰剂。
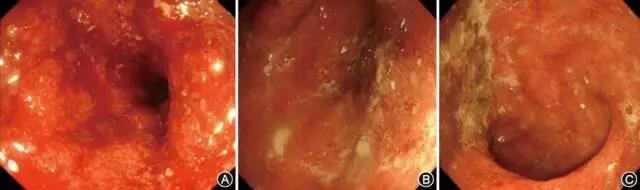
背景和目的:肠外甲氨蝶呤可使UC临床症状缓解,但是不能改善内镜下的黏膜炎症。研究者进行了一项随机安慰剂对照试验,旨在评估经甲氨蝶呤和糖皮质激素诱导治疗后,无激素应答或缓解的UC患者,肠外甲氨蝶呤治疗的有效性。
方法:研究者于2012年2月~2016年5月进行了一项为期48周的试验,研究对象为179名尽管既往接受了传统或生物治疗但病情仍为活跃性的UC患者(梅奥评分为6~12分,内镜子评分≥2)。研究包括16周的开放标签甲氨蝶呤诱导期,之后是32周的双盲安慰剂对照维持期。患者皮下注射甲氨蝶呤(25mg/周),以及12周逐渐减量的糖皮质激素。16周时,无激素应答者随机分配到继续甲氨蝶呤(25mg/周,44人)或安慰剂(40人)的组中,直到48周。研究者通过分析48周时不使用糖皮质激素或其他药物控制疾病活跃度而仍能保持无复发和处于缓解的患者比例,比较了治疗有效性。
结果:91名患者(51%)在16周时实现应答,84名患者纳入到研究维持阶段。该阶段,安慰剂组60%(24/40)的患者,甲氨蝶呤组66%的患者(29/44)UC复发(P=0.75)。48周时,安慰剂组30%(12/40)的患者,甲氨蝶呤组27%(12/44)的患者无激素临床缓解但不需要额外治疗(P=0.86)。未检测到甲氨蝶呤新的安全性问题。
结论:在预防诱导治疗期实现无糖皮质激素应答患者的UC复发上,肠外甲氨蝶呤(25mg/周)不优于安慰剂。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#肠外甲氨蝶呤#
47
#GAS#
36
#Gastroenterol#
36
#溃疡性#
38
#AST#
43
#无应答#
41
#Gastroenterology#
38